As we kick off 2023, it is hard to believe only a year has passed since the federal government approved California’s ambitious plan to transform the Medi-Cal program. The initiative, CalAIM (California Advancing and Innovating Medi-Cal), is a multi-year effort to advance person-centered, holistic care for people with complex needs, while also pursuing population health goals to make care more equitable for everyone in Medi-Cal.
CalAIM is so important and far-reaching that it obliges all of us to work together in new ways to realize its promise. So, let’s review how much CalAIM has already undertaken and peer over the horizon at what is still to come.
First, the accomplishments. Countless people across California’s Department of Health Care Services (DHCS), health systems, provider groups, health plans, community-based organizations, and county health departments came together to ensure a smooth transition for tens of thousands of Medi-Cal enrollees who were supported by CalAIM’s precursor programs, known as Whole Person Care and Health Homes. This alone was a huge lift.
In addition, California achieved the following:
- Launched a new benefit — Enhanced Care Management (PDF) — for key populations of focus statewide
- Commenced the novel approach of managed care plans offering up to 14 non-traditional services, such as connecting people to housing or asthma remediation, through Community Supports (PDF)
- Instituted a No Wrong Door (PDF) policy, allowing Medi-Cal patients to receive mental health services regardless of where they initially seek care, and allowing providers to be reimbursed for that care
- Laid the groundwork for contingency management pilot programs in 24 counties, which are set to start in early 2023 under the name “Recovery Incentives.” Contingency management is an effective treatment for methamphetamine.
And that is just a partial list.
The main strategy that CalAIM employs to move a fragmented care system to a person-centered system, and to do so with sustainable funding, is managed care. Managed care is not perfect, and it brings with it an additional layer of administrative requirements. But given all the trade-offs, it is probably the best tool we have to ensure that the whole-person care Californians need can be delivered equitably.
It is important to remember that CalAIM has inherently required everyone involved to build the bridge while crossing it. It involves countless new partnerships, myriad new data sharing needs, uncertain referral volume, and cash-flow constraints introduced by retrospective payments — all at the same time. To get this far has been an enormous lift across the entire Medi-Cal system. And all this change has taken place on the heels of a once-in-a century pandemic.
Yet we need to keep our eyes on the mountaintop in the distance. CalAIM offers an unprecedented opportunity to make Medi-Cal and other safety-net programs work better for the Californians who depend on them. It’s a chance to make care more equitable and easier to access. Beyond that, it enables transformation of health care delivery to meet the needs of the whole person wherever people go for care. For example, a person who has a stroke needs their immediate health crisis addressed but may also need paid assistance at home to fully recover. So much of Californians’ ultimate well-being hinges on factors outside the health system, and many programs in CalAIM are designed to help address these social needs, particularly for people with complex physical and behavioral health conditions.
And for the millions of people with health needs that are less complex, CalAIM raises the bar on quality, access, satisfaction, and equity (PDF). DHCS is making variation in quality metrics more transparent (PDF) and imposing fines on managed care plans falling short on key measures.
What to Expect in 2023
CalAIM brings a raft of new possibilities and challenges in 2023. Across the state, people will be working on instituting:
- Population Health Management initiatives that will enhance proactive and equitable care for all Medi-Cal members, not just those with complex needs, and add new populations of focus for Enhanced Care Management
- A more seamless system for seniors and people with disabilities that features managed care plans taking responsibility for institutional long-term care
- Standardized screening tools for every behavioral health entry point to minimize provider confusion
- Behavioral health payment reform (PDF) so that billing for these services mirrors the system for physical health billing
Again, this is just a partial list. There’s also news to come on additional waiver requests: the California Behavioral Health Community-Based Continuum Demonstration waiver and “pre-release services” for people leaving jails and prisons.
What do all these programmatic changes have in common? They support a deepening of engagement with people who for too long have not been well-served — or not understood by — the system. The goals of these changes are to improve health equity for all Californians. The changes support a more rational and consistent delivery of Medi-Cal services to enrollees in every corner of the state. And they support more reliable funding streams for service providers.
From the patient or consumer perspective, CalAIM should streamline the system to make it easier for people to get the care they need. Initially, it may not feel like an improvement to providers, health plans, county health departments, and other players in the health care system. Indeed, the operational complexities of moving from one established system to a new way of doing business should not be underestimated. And it takes time to cultivate cross-sector collaboration, trust, and relationships.
Building the Infrastructure for People-Centered Care
It would be nearly impossible to implement CalAIM successfully without making other improvements to the system. That’s why CalAIM makes key investments around data exchange, health workforce, and the infrastructure to sustain new partnerships. Exchanging data among health care systems and social services agencies is really the only efficient way for different providers to obtain a unified view of the patient as a whole person with complex and interconnected health needs. The state has set a 2024 deadline for most health care providers to be able to share health care information. This year’s state budget includes $250 million to support data exchange adoption.
Much of CalAIM relies on managed care organizations, but their key on-the-ground partners — community-based organizations, hospitals, clinics, county agencies, tribes, and other providers — need to hire and train staff and build infrastructure if they are to participate successfully. Of course, that all takes money. DHCS has allocated $1.85 billion in a new program called Providing Access and Transforming Health for these organizations to build up their community-based workforce and systems to be effective partners with managed care organizations in reaching people who too often have been left behind. DHCS announced in late December that it will contract with five commercial health plans in California. This move finalizes which health plans will operate in each county starting in January 2024 so that plans and providers can continue working together to implement CalAIM programs.
CHCF is proud to partner with everyone across the state working to make the CalAIM vision a success. Momentous changes like this take time. It’s worth remembering other challenges that California has met. Ten years ago, 22% of Californians were uninsured. Today it is less than 6%, thanks to California’s enthusiastic embrace of the Affordable Care Act and additional Medi-Cal coverage expansions. In 10 years’ time, we hope to see a statewide health system that responds to all in a person-centered and equitable way. If any place can do this, it is California.
Authors & Contributors

Melora Simon
Associate Director, People-Centered Care, California Health Care Foundation

José Luis Villegas
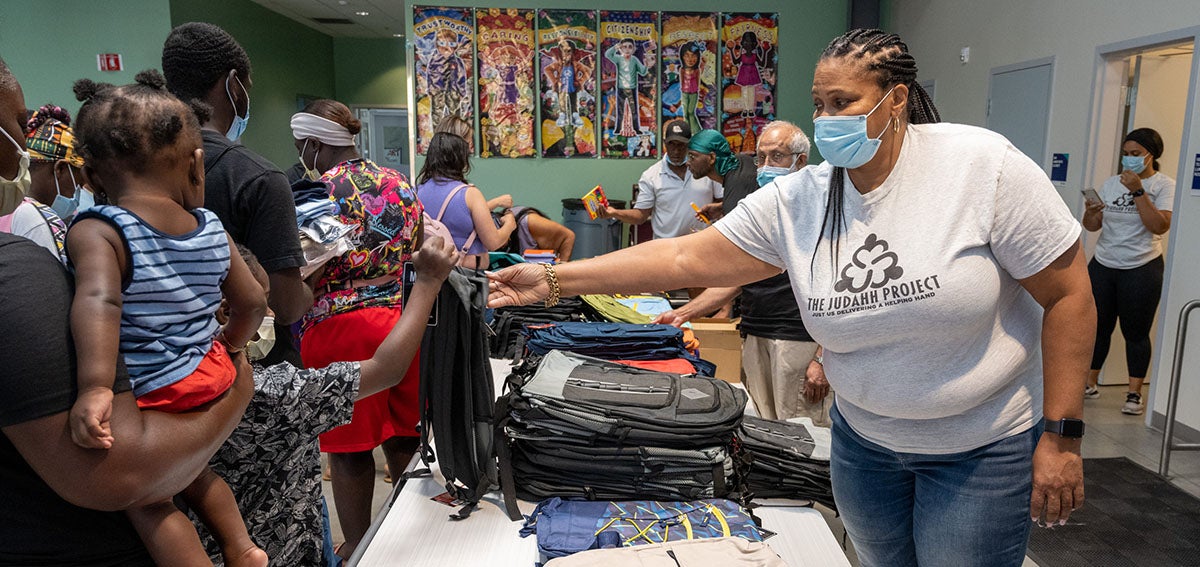
José Luis Villegas is a freelance photojournalist based in Sacramento, California, where he does editorial and commercial work. He has coauthored three books on Latino/x baseball. His work appears in the Ken Burns documentary The 10th Inning and in the ¡Pleibol! exhibition that debuted at the Smithsonian Institution’s National Museum of American History and has been appearing at museums around the country.
Villegas’s work has been exhibited at the Museum of Fine Arts-Houston; the Baseball Hall of Fame in Cooperstown, New York; and at the Oakland Museum of California. Villegas also works as a medical photographer at Shriners Hospital in Sacramento.





