|
Getting your Trinity Audio player ready…
|

CHCF’s leader delivered opening testimony at a Jan. 27 Assembly Health Committee informational hearing on how federal budget cuts could affect California’s health care system. Her full remarks are below.
Good afternoon, Madam Chair, Mr. Vice Chair, and Members of the Committee.
I am Dr. Sandra Hernández, President and CEO of the California Health Care Foundation. For those who don’t know us, we are an independent, nonprofit philanthropy. Our mission is simple: We listen to Californians, we analyze data, and we work with partners across the state to improve the health care system so that it works for everyone.
We are meeting in a volatile time. The news coming out of Washington is daunting. But I want to be clear: while the federal landscape has shifted, California has enormous power to mitigate the damage — and to protect the health of our people.
California’s Values
Regardless of federal policy, California has a long tradition of taking care of its own.
In California, we do not view health care as a luxury. We see it as a fundamental necessity for all. We see this in poll after poll: Californians want a system where people can get care when they need it, without facing significant financial barriers to care, including the fear of bankruptcy. These are not just beliefs. We have a legacy that we should all be proud of, and that we must defend today.
What We Are Defending
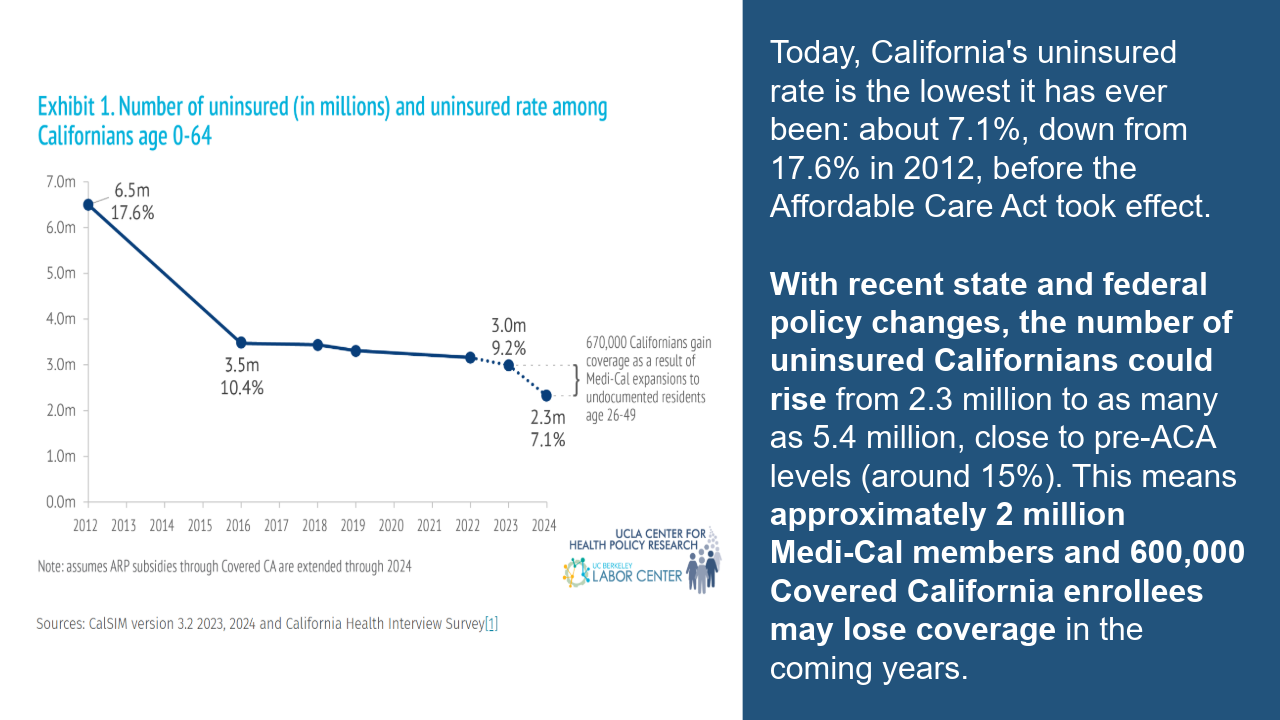
Because of the work done in this building, California has made historic progress toward universal coverage. You can see the dramatic decline in uninsured rates in this chart.
We built a Medi-Cal system that today covers half of the children in this state. It covers one in five working Californians. It supports millions of seniors and people with disabilities. We built a system that prioritized inclusion.
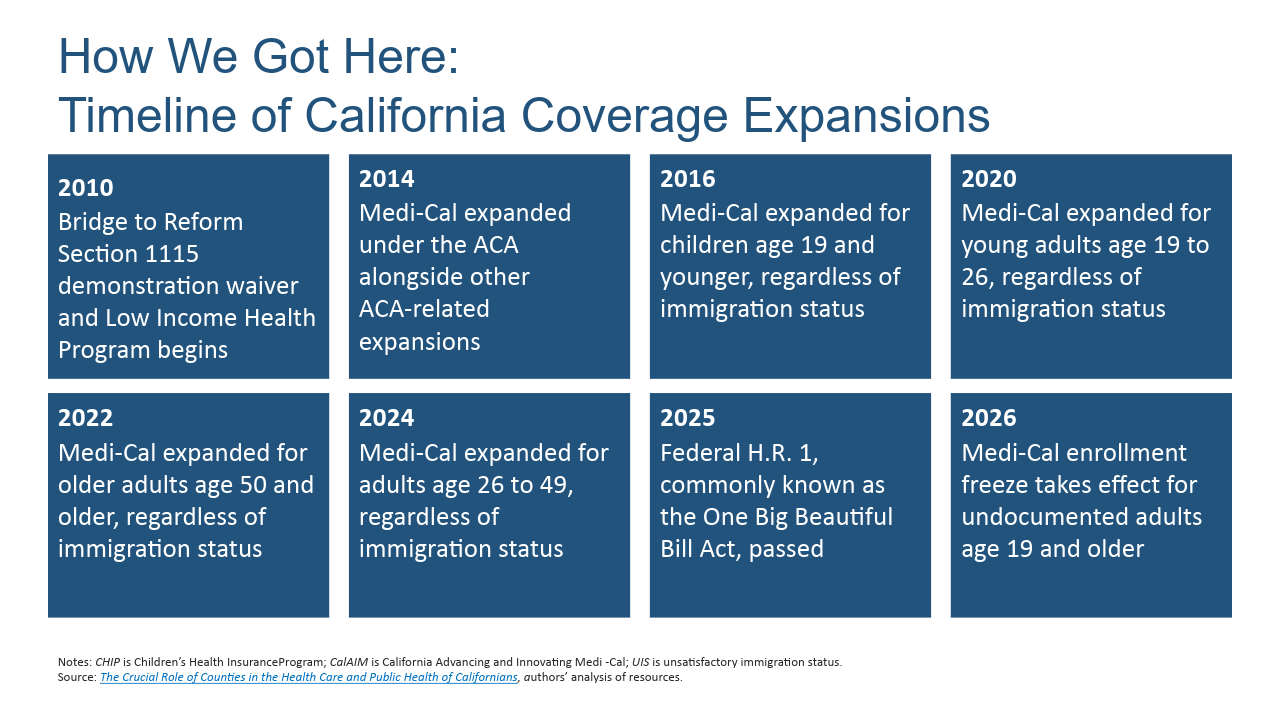
I’ve included a full timeline of coverage expansions so you can see how we got here.
The Threat: Implications of H.R. 1
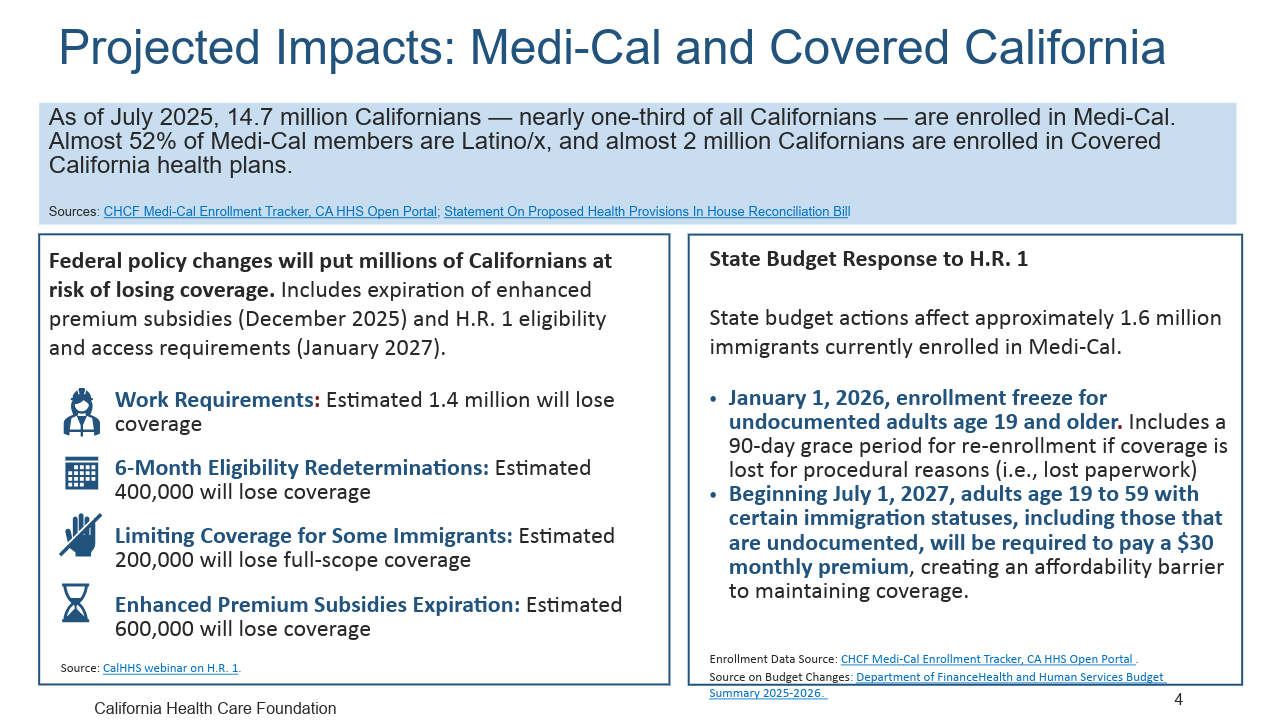
Today, we are defending the health security of nearly 15 million Californians against the largest funding reduction in the history of the Medicaid program.
The threats posed by H.R. 1 come in different forms.
First, the financial cliff. H.R. 1 cuts federal funding for health care by $1 trillion nationally over the next decade. For California, we estimate this translates to tens of billions of dollars in annual cuts. As you are all aware, that is a hole in our budget that we cannot simply fill with state reserves.
Second, the administrative wall. The introduction of work requirements and six-month eligibility redeterminations — is often framed as a policy about work. It is not. It is a policy about paperwork. We are looking at a scenario where otherwise eligible working parents lose their coverage simply because they couldn’t navigate a complex verification process in time.
Third, the attack on immigrant families. Starting Oct. 1, 2026 (this year), H.R. 1 excludes huge populations of immigrant Californians from coverage. But the damage starts sooner than that. We are already seeing the “chilling effect.”
When families are terrified of deportation and family separation, they go underground. They avoid clinics. They skip appointments for their eligible U.S. citizen children. And as a result, preventable health problems become emergencies. This is bad for patients, providers, and taxpayers.
The pain extends to the middle class as well. By failing to renew federal premium subsidies for the individual market, the bill will cause monthly premiums to skyrocket for 2 million Californians who buy their own insurance through Covered California, forcing many to drop coverage entirely.
Finally, I want to acknowledge that you have had to make some hard decisions due to state budget constraints. To date, that has included freezing Medi-Cal coverage for undocumented immigrants, imposing a $30 per month premium on immigrants who maintain Medi-Cal coverage.
Four Imperatives for California
So, where do we go from here? I believe this crisis presents California with four distinct imperatives to meet this moment — to not just defend what we have, but to adapt and strengthen our system for the future.”
No. 1: Minimize the harm of work requirements. If we cannot stop the federal mandate, we must minimize the friction. The state must move aggressively to automate verification. We have the data systems to know who is working; we should not put the burden of proof on someone who is working two jobs, or experiencing homelessness. We also need trusted messengers on the ground, like community health workers, to help people manage this new reporting burden.
No. 2: Make sure the uninsured can access care. We must confront the reality that under H.R. 1, the number of uninsured Californians will rise. For these residents, our priority must shift to ensuring access to care until universal coverage is possible. To do this, we need to revisit the safety net strategies of the pre-Affordable Care Act era. Back then, we navigated a patchwork system where eligibility, covered services, and payment models varied from county to county resulting in different levels of access and care across the state This is an opportunity to avoid that fragmented system of care. One big question today is whether the state or counties should lead the way. My advice is to study what worked in pre-ACA local programs and use what we learn to create a standardized, scalable framework that all counties can implement. This framework should emphasize what we know works — prevention and primary care, continuity of care, and administrative simplicity.
No. 3: Rethink the future of Medi-Cal. We cannot simply patch the immediate holes created by H.R. 1. We also need to strengthen Medi-Cal for the long term. The program is a vital lifeline, but it is also a massive, complex program that was built piece-by-piece over 60 years. While the current system has served us well, it requires significant structural reform to take us where we need to go for the next decade and beyond.
That is the work of the Future of Medi-Cal Commission, which had its first meeting last week. I have deep confidence in the experienced leaders serving on this commission, and I believe they will be valuable partners to this committee as it completes deliberations later this year.
No. 4: Use regulatory authority to contain costs. Finally, California must get serious about making health care more affordable.
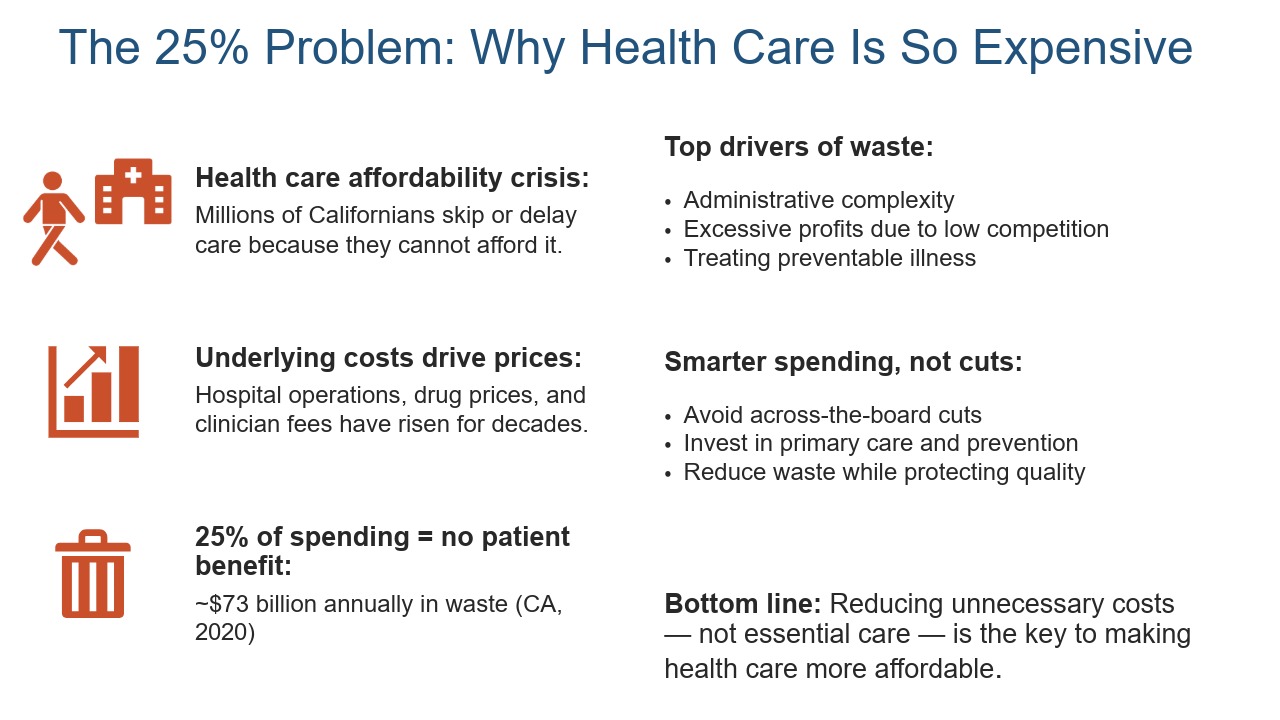
We estimate that 25 cents of every health care dollar is wasted on administrative complexity, on incompatible data systems, and on preventable illness. We cannot afford that anymore. The Office of Health Care Affordability gives the state an incredibly important lever for change. As a member of its board, I am committed to ensuring that every dollar the state, employers, and consumers are spending is buying high-impact care.
One side note: I strongly believe that technologies like AI, data exchange, and telehealth can help us do all the things I mentioned much more effectively — and more cost-effectively. Technology should be central to any strategy going forward.
‘In This Together’
I want to close with this thought: We are all in this together.
There is an urgent need for all stakeholders to set aside their unique perspectives and to come together for the well-being of Californians.





