- Identify a partner champion motivated and committed to addressing key gaps in care
- Ensure the proposed activity will meaningfully benefit the partner service line
- Start small and build
- Embed project tools, processes, and metrics into electronic health records and workflows
- Align project objectives with larger administrative goals
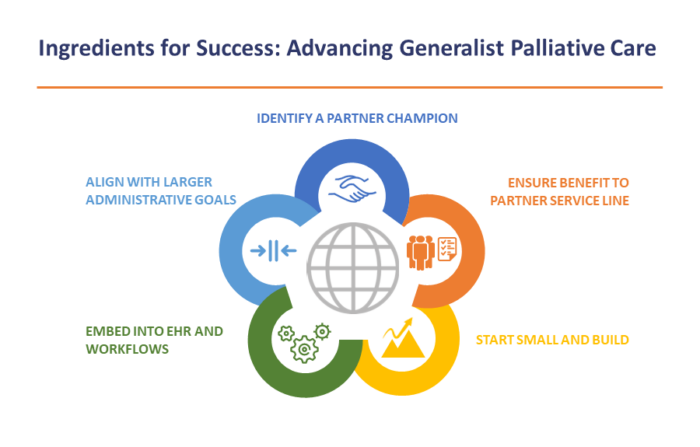
While each ingredient is important individually, together they increase the potential for project adoption and sustainability.
1. Identify a partner champion motivated and committed to addressing key gaps in care.
Identifying an enthusiastic partner champion and target audience is consistently reported as the top recommendation for health systems considering implementing generalist palliative care projects. Effective integration requires palliative care and partner service line collaboration and a clear focus on a specific quality gap and behavior change built within existing workflows. (See Needs Assessment sections 1–3) Successful partner service line and palliative care partnerships happen because the two service leads identify a shared quality gap to close or an opportunity to improve care in the partner service line by applying generalist palliative care skills.
“It’s really about the champions and choosing the right people who are interested in the project. If the service line is not interested in the project, it’s going to get pushed down to the bottom of their list. The biggest success was finding people who took the project and ran with it.”
—Palliative care lead
“It’s really about the champions and choosing the right people who are interested in the project. If the service line is not interested in the project, it’s going to get pushed down to the bottom of their list. The biggest success was finding people who took the project and ran with it.”
—Palliative care lead
Challenge: One challenge experienced in implementation includes shifting priorities within the partner service line. New organizational priorities and demands on the service line members’ time, staffing changes, or other unforeseen circumstances (like what CHCF teams experienced with COVID-19) may necessitate revisiting the partner service line commitment, project scope, and timeline. Flexibility is important as the environment changes and adjustments need to be made. Reviewing priorities, adjusting timelines, revising scope, or reframing goals can help continue the momentum while recognizing the new priorities or time limitations of the partner.
In some cases, it might be appropriate and necessary to change gears and find a ready and willing champion in a different service line. For example, changes in the environment may increase interest and readiness in other service lines — this was the case for some CHCF teams in response to COVID. Because the pandemic disproportionately affected people with low incomes and many communities of color — populations served by public health care systems — some service lines felt an urgency to improve their palliative care skills, such as having conversations about goals of care or making sure patients understood their prognosis to help them avoid unwanted hospitalizations.
2. Ensure the proposed activity will meaningfully benefit the partner service line.
Palliative care practitioners strive to “meet patients where they are.” This same approach is essential for engaging partner service lines in generalist palliative care work. It is important for the target audience to view the intervention as meaningful and worth their efforts and to be open to learning new skills. For example, a partner service line may identify the need to improve the quality of primary pain management and to reduce pain-related treatment delays for patients. Giving the target audience a variety of tools (e.g., communication skills, assessment and documentation workflows, metrics to monitor progress) to help solve a problem they have, combined with consultation and mentoring from the palliative care team, increases engagement and adoption.
See the Needs Assessment section for tools to identify gaps, define the desired behavior change, and clarify factors that predispose, enable, and reinforce that target behavior. These processes help teams plan an intervention that will stick.
“Advance care planning was not the area of palliative care that was most interesting to me before we started this . . . (though) I do think it’s incredibly important and obviously has broad reach. But I think it was just partner service line lead interest and demonstrated initiative that made me focus on it for this project.”
—Palliative care lead
“[Partner service line] residents have not had communication skills training in the past, but they wished they could lead goals of care meetings more effectively and feel confident providing end-of-life care. So we provided CAPC [Center to Advance Palliative Care] modules, a series of lectures which included a simulation case, and some curbside consultations from the palliative care lead.”
—Partner service line lead
Challenge: Progress can be impeded if the processes that support the desired behavior change are not fully integrated into partner service line workflows and operations right at the beginning. As an early step, palliative care and partner service line partners should work together to build the desired behavior changes into the current workflows and documentation processes and identify and engage the right staff. Regular meetings — weekly, biweekly, or monthly — are important to monitor progress, troubleshoot, and adjust as needed.
3. Start small and build.
Promoting behavior change slowly and incrementally, with a detailed focus, was universally identified by CHCF teams as critical for implementing a generalist palliative care project. Keeping a project focus intentionally narrow and well-defined — for example, training residents to document pain assessments and treatment plans — helps ensure the behavior change is manageable and sustainable. This enables teams to test the new processes, such as new workflows and new documentation processes, and adjust and revise them as needed. Starting out small, with a clear target, helps teams lay a solid foundation for their work, and they can build from there.
“We used a very different take on the goals of care serious illness conversation. We focused on micro-conversations that happen over time (‘microdosing goals of care’). We had small conversations, and as we got to know patients we would ask, ‘Do you have a surrogate decisionmaker? Have you ever thought of this? Let’s touch on this next time.’ We folded these small goals of care nuggets into our clinic visits to make the conversations more sustainable and part of routine practice. I do think that was a big change.”
—Partner service line lead
Challenge: Starting too big or too broad is a common challenge. Targeting too many different types of staff for behavior change can be a challenge, given the variety of workflows, roles, and intervention approaches for different staff members. Behavior change work should be specific and targeted for a defined group so that new skills and approaches can be applied, tested, and revised as needed. Similarly, it is helpful to start with a well-defined group of patients targeted for the intervention. This can help the team track the impact and effectiveness of the intervention before spreading it more broadly.
4. Embed project tools, processes, and metrics into electronic health records and workflows.
It is important to embed the processes that support the desired behavior change into existing workflows and systems to support sustainability. Palliative care and partner service line teams should collaborate to examine the workflows and the “pain points” to address. For example, teams might opt to embed documentation tools or phrases in current electronic health record (EHR) templates or integrate educational sessions on the desired behavior change into existing trainings. Making time to understand the unique needs and workflow of the partner service line at the outset, and when possible, working with information technology (IT) experts on integrating automated or supportive documentation and tracking functions into the EHR can help teams sustainably integrate these behaviors into the day-to-day work of partner service lines.
“ACP [advance care planning] doesn’t have health care maintenance standards like these other screenings, but we added it to a health care maintenance dashboard that they already use.”
—Palliative care lead
Challenge: While critical for sustainability, modifying the EHR to support generalist palliative care (e.g., documenting advance care planning conversations and workflow, integrating a validated pain assessment tool) can be a challenge. While some teams can get an IT analyst to assist them, many systems are challenged to have enough IT staff to support new development. IT analysts may be busy, unavailable, have other priorities, or may not understand how to make the requested changes. Those unable to get IT support should consider creative ways for tracking and be flexible in approaching development of the tracking system. Teams can sometimes improvise approaches, such as integrating templated text (e.g., “dot phrases” in Epic) and intervention documentation tools into EHR platforms.
“Lack of IT support impacted our project in many ways. It necessitated project data evaluation that did not rely on automated reporting within Epic. We created SmartLists and worked with (specialty) team members to maintain team dot phrases and integrate documentation elements as mineable fields within note templates.”
—Palliative care lead
5. Align project objectives with larger administrative goals.
Understanding the health system’s top goals and priorities can help to both motivate the adoption of palliative care in partner service lines and secure needed resources. For example, California public health care systems are currently participating in the Quality Incentive Program (QIP), a pay-for-performance program where payments are linked to achievement of performance on a set of quality measures for Medi-Cal managed care enrollees. One of the optional QIP measures focuses on advance care planning. Organizations that have elected this measure have a strong incentive to improve approaches to engaging patients in advance care planning conversations.
Health systems may also be motivated to align their care practices with the recommendations of clinical specialty associations that encourage integration and promotion of palliative care. For example, the palliative care bundle of the American College of Surgeons Trauma Quality Improvement Program can help encourage adoption of palliative care skills in trauma surgery. Both the American Society of Clinical Oncology and the American College of Cardiology have clinical practice guidelines or recommendations on the integration of palliative care into standard care for people with cancer and heart failure, respectively.
Finally, to sustain commitment from organizational leaders and to engage additional service lines to spread palliative care processes across the system, teams must share information on their progress and impact (see “Measuring Impact and Making the Case”).

