Health care leaders are asked to demonstrate how internal organizational diversity, equity, inclusion, and belonging (DEIB) investments impact community health equity outcomes. To answer this question, the California Improvement Network (CIN) conducted a comprehensive environmental scan of academic literature, expert knowledge, and case studies of health care organizations.
The environmental scan showed that there is a notable shift from assessing impact of DEIB programs with narrow profit-driven ROI metrics toward recognizing that anti-racist organizations create broader cultures of health equity. Exemplar organizations that are moving the needle on health equity consistently do the following:
- Understand that the root causes of inequities – structural racism, intergenerational trauma, marginalized treatment, and disparities in wealth and education – occur within organizations as well as in the broader communities served.
- Begin from the premise that organizational DEIB and health equity outcomes are interdependent; to address root causes of health disparities, systemic interventions must create “cultures of equity,” which means enacting commitments and methods for all patients, employees, and communities to individually and collectively identify and work to transform organizational dynamics that lead to inequities.
- Fully commit to invest in both organizational DEIB and health equity initiatives centered on improving patient and community outcomes.
Below we illuminate three strategic insights to help health leaders and teams build a shared understanding and develop cultures of equity.
“Comprehensive organizational efforts like ours are costly. At the same time, that cost is necessary to eliminate the overwhelming moral and economic costs associated with structural racism, including preventable medical expenses, illnesses, and premature deaths that disproportionately affect communities of color.”
– Critical Theory, Culture Change, and Achieving Health Equity in Health Care Settings, University of Chicago Medicine, 2022
Reframing the business case for DEIB
The demand for health equity leaders to prove the worth of organizational DEIB investments can be linked to non-health care industry specific literature composed of generalist think pieces and studies from large corporations focused on how to make the “business case” for DEIB.
This literature champions diversity, equity, and belonging as a top-down investment in corporate business models that use company performance ROI metrics such as productivity, competitive advantage, employee retention, shareholder primacy, and bottom-line profit to determine organizational DEIB is a worthwhile investment.
However, there is a growing critique that prioritizing these measures is problematic because research continues to demonstrate that racial and gender inequality in the workforce is directly tied to corporate governance designed to maximize traditional ROI metrics.
This critique is part of a call to ground organizational DEIB interventions in broader systemic change. While the literature on building a business case for DEIB often defaults to corporate governance business models, emerging social impact business models and community-based organization models demonstrate ways to expand beyond profit-driven metrics toward value-centered metrics. These models use root-cause solutions that redesign organizational structures, transform organizational hierarchy, address power imbalance, and shift misaligned financial incentives to create accountability structures that benefit all.
“In a culture of equity, all employees – individually and collectively – identify and reflect on the organizational dynamics that reproduce health inequities and engage in activities to transform them.”
– Create Cultures of Equity: Advancing Health Equity Roadmap
Moving beyond ROI to value-based equity metrics
While health care organizations have often defaulted to using profit-driven ROI metrics to prove the value of DEIB investments, upstream-focused health equity initiatives are shifting to value based metrics, such as Social Return on Investment (SROI) and Value on Investment (VOI), to more appropriately and effectively measure health equity and community impact.
Organizations and initiatives including HealthBegins, Rush University Health System’s Anchor Strategy, and the University of Chicago Medicine’s Urban Health Initiative are exemplars of how to go beyond ROI and utilize SROI and VOI metrics as a bridge to building cultures of equity. These bridging metrics enable health equity leaders to adopt metrics designed to measure, optimize, and accelerate health equity interventions across organizations and communities.
“Measuring the impact of DEI efforts on patient outcomes is critical. However, ameliorating and eliminating root causes of health inequities is a complex endeavor. Organizations should carefully consider the applicability of the measures they choose to evaluate the progress of equity-focused initiatives. Many measures (e.g., return on investment, reduced costs) associated with the contemporary economic zeitgeist and traditional biomedical health perspectives ignore the potential impact of culture change and the lengthy timelines needed to align equity-focused initiatives across policy sectors. Such measures may create barriers for the long-term visionary, courageous, and experimental efforts needed to achieve health equity.”
– Critical Theory, Culture Change, and Achieving Health Equity in Health Care Settings, University of Chicago Medicine, 2022
Deepening collaboration and community learning to create cultures of equity
National programs, including IHI’s Health Equity Initiative, the Healthcare Anchor Network, and RWJF’s Advancing Health Equity, are playing a crucial role in developing health equity frameworks, guides, and learning collaboratives that are paving the way for health care organizations to create cultures of equity.
Highlighted here is the work of University of Chicago Medicine as an exemplar for health leaders to learn from as they work toward creating cultures of equity across their organizations and communities served.
Following 10 years of progress implementing their DEI theory of change and comprehensive operational and community health equity transformation work, University of Chicago Medicine summarize their efforts in “Critical Theory, Culture Change, and Achieving Health Equity in Health Care Settings.” Instrumental is how their theory of change, strategy, operations, and collaborations supports this shift. Their five interconnected strategies that have improved patient outcomes, patient-provider interactions, organizational dynamics, operational processes, clinical education, and community relations are:
- Strategy 1: Deliberately ground diversity, equity, and inclusion (DEI) in critical theory, which questions the dominant forms of thinking by challenging normative and assumed power relations.
- Strategy 2: Ensure training goes beyond cultural competence and humility to include critical consciousness, which is the ability to critically analyze organizational and societal conditions that produce health inequities so they can directly transform them.
- Strategy 3: Strengthen growth-fostering relationships so they can be vehicles for change.
- Strategy 4: Empower an implementation team that embodies and models a culture of equity.
- Strategy 5: Align equity-focused culture transformation with equity-focused operations transformation to support transformative praxis within organizational walls and throughout communities they serve. (Praxis is defined as a process of reflection and action based on critical analysis.)
See the graphic below to better visualize how these five strategies function to achieve health care equity.
In recognizing that organizational DEIB programs create and strengthen cultures of equity for all, health care organizations can expand beyond traditionally narrow ROI metrics to interdependent community health outcomes. This can empower health leaders to have a greater upstream impact on the health of communities.
As you digest this work and resources, consider, “How is your organization embodying a culture of equity?”
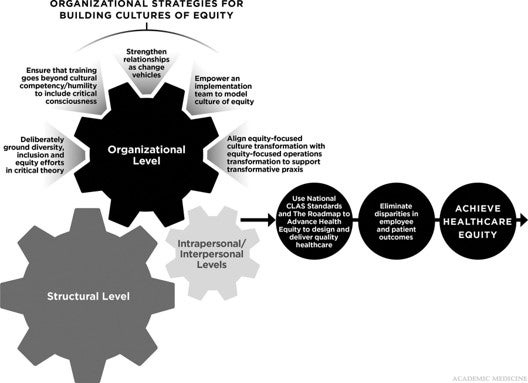
Organizational Strategies for Building Cultures of Equity graphic. Copyright © 2021 by the Department of Diversity, Equity, and Inclusion, University of Chicago Medicine.
The California Improvement Network (CIN) is a learning and action community that advances equitable health care experiences and outcomes for Californians through cross-sector connections, spreading good ideas, and implementing improvements. Learn more about the California Improvement Network, a project of the California Health Care Foundation that is managed by Healthforce Center at UCSF, and sign up for the CIN newsletter.


