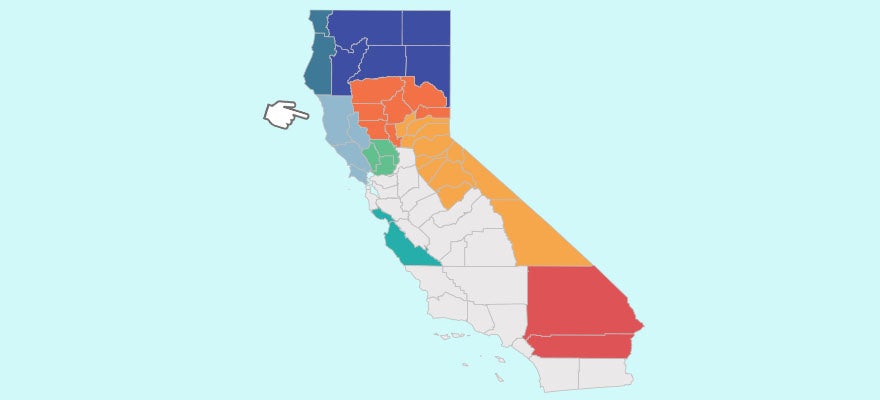
Around 80% of Medi-Cal members are enrolled in a Medi-Cal managed care plan. CHCF has focused on tracking trends in the quality of care overseen by these plans. It has also closely followed the state’s recent process to select and write new contracts with Medi-Cal managed care plans, noting the once-in-a-decade opportunity to hold these plans to higher standards for access and quality.

Six Things to Watch For Now That Medi-Cal Has Picked Commercial Managed Care Plans
Continued investment and sound implementation will lead to higher quality care for millions of Medi-Cal enrollees — and progress toward reducing racial and ethnic disparities in outcomes.

A Golden Opportunity to Narrow California’s Racial Health Disparities
The state now has a rare opportunity to force health insurers to do more to improve the care that people with low incomes receive through Medi-Cal.

A Close Look at Medi-Cal Managed Care: Stories of Quality Improvement Success
This paper highlights examples of Medi-Cal managed care plans that have made significant progress on individual quality-of-care measures. The paper identifies several common, interconnected strategies that were key to improving quality and provides concrete examples of how plans put these strategies into place.


Paying Medi-Cal Managed Care Plans for Value: Design Recommendations for a Quality Incentive Program
This report recommends a new way to pay Medi-Cal managed care plans (MCPs) designed to improve the quality of care for Medi-Cal enrollees. The Department of Health Care Services would withhold part of its capitation payments to MCPs, who could earn back some or all of the amount withheld depending on their performance on quality…