
If the first week of 2021 is any indication, the COVID-19 pandemic will continue to batter California and the nation well into the new year. Two vaccines are authorized for emergency use in the US, and many more vaccine candidates are moving through the pipeline. But the early phase of the nationwide vaccination campaign — an effort of unprecedented scale and complexity — has been sluggish. While federal officials stated a goal of giving 20 million Americans the first of two doses by the end of 2020, they achieved only 14% of that goal, the New York Times reported.
California, once praised for its aggressive moves to stave off the spread of the coronavirus, remains a hot spot for deaths, hospitalizations, and new cases — especially in Southern California. Across the state, intensive care unit (ICU) capacity is at an all-time low, and efforts to close health equity gaps have been blotted out by a relentless post-holiday surge.
The discovery of a new variant of the coronavirus in the United Kingdom is adding fuel to the fire. While mutations in viruses are normal and expected, the new B.1.1.7 variant appears to be more contagious, underscoring the need to rapidly increase vaccination rates.
Desperate Governors
Just a few weeks after vials of the COVID-19 vaccine began making their way across the country, efforts to inoculate Americans are way behind schedule. “Desperate governors are facing a vacuum of federal support, along with dire funding and workforce shortages that are hampering the pace of the rollout,” Rachel Roubein, Brianna Ehley, and Sarah Owermohle reported in Politico.
The federal government distributes vaccine doses to states weekly, but states are responsible for allotting those doses to local health jurisdictions, which in turn coordinate vaccine allocation with health care providers in their areas. Public health experts say this complex distribution process further burdens overworked and understaffed county public health agencies.
“Health departments are right now multitasking — they’re still doing testing and contact tracing, along with planning for the vaccines and actually giving the vaccines,” Glennah Trochet, MD, deputy public health officer for Nevada County, told Sammy Caiola in Capital Public Radio.
Health care providers play an essential role in getting the doses into people’s arms, but large numbers of quarantined health workers compound workforce shortages that existed before the pandemic. In California’s San Joaquin Valley, hundreds of local health care workers are quarantined due to infection or exposure to COVID-19. The remaining providers must juggle the tasks of tending to the surge of COVID-19 patients, administering vaccine doses, and monitoring people for adverse reactions in the 15 minutes post-vaccination.
So far, California has received 2.1 million vaccine doses. But as of January 9 the state had only administered about 32% of the doses. At a January 4 press conference, Governor Gavin Newsom said, “The first 10, 15 days we’re going to slowly start building pace . . . you’re going to start seeing more rapid distribution of this vaccine, I can assure you that.”
To accelerate distribution, the California Department of Consumer Affairs recently issued a waiver (PDF) allowing dentists to administer the COVID-19 vaccine. The California Department of Public Health revised its vaccine prioritization guidelines to allow local health departments and providers to immunize people in lower-priority groups if all opportunities to immunize willing people in the current prioritized tier have been exhausted. On January 8, Newsom proposed spending an additional $300 million or more to assist with the vaccine rollout.
California COVID-19 Deaths Surpass 29,000
California’s winter surge is holding steady at levels sharply higher than the peak in the middle of last year. State health authorities reported a record one-day total of 695 deaths from COVID-19 on January 9. The “daily coronavirus case tallies remain around four times what they were during the state’s summer surge, and officials predict that the aftereffects of a December surge linked to holiday gatherings will worsen as the winter drags on,” Lucy Tompkins, Mike Ives, and Julie Walton Shaver reported in the New York Times.
As of January 10, California had more than 2.6 million confirmed cases of COVID-19 that led to 29,701 deaths. These may be undercounts. According to the COVID-19 Tracking Project, major US holidays often lead to delays in data reporting. “Given that New Year’s holiday weekend will also cause data disruptions, we aren’t expecting a return to normal reporting until closer to the middle of January,” the project website states.
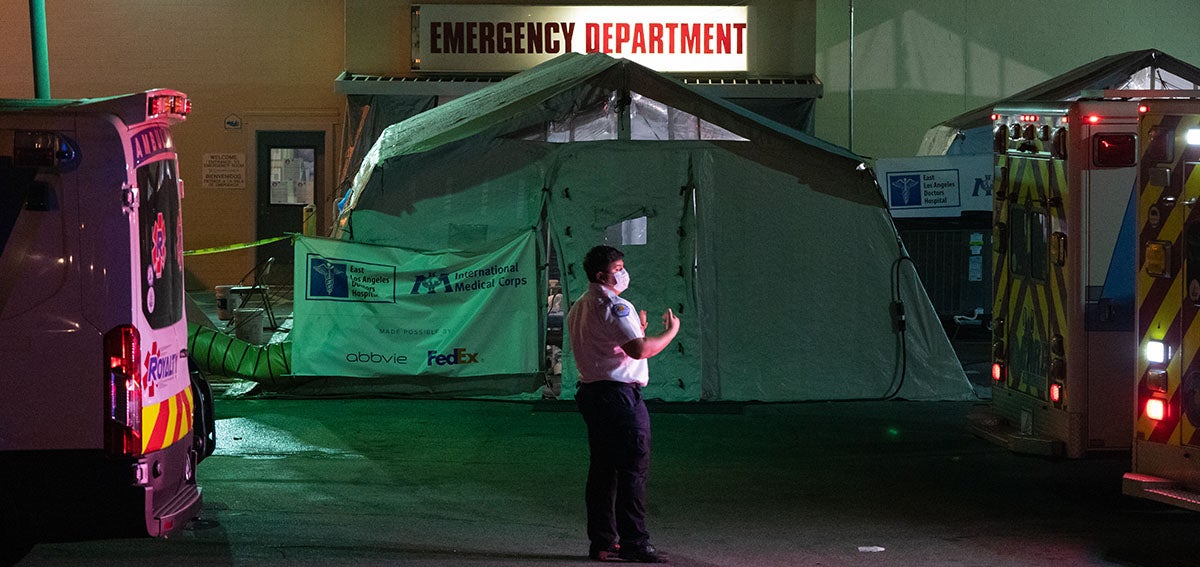
Unlike its previous surges, California is experiencing alarmingly low capacity of licensed ICU beds. Southern California and San Joaquin Valley are at 0% ICU bed capacity, the Bay Area is at 3%, Greater Sacramento is at 6.4%, and Northern California is at 27.5%, according to a Los Angeles Times tracker.
“My biggest impression when I look at these numbers is just fear,” Peter Chin-Hong, MD, an infectious disease expert at UCSF, told Jason Fagone in the San Francisco Chronicle. “You can have the best therapy in the world, [but] if you have a lot of people come in, you just can’t take care of them all in the same way.”
Paramedics in Southern California have been instructed not to transport patients to the hospital who have little chance of survival, Jaclyn Diaz reported for NPR. And the Los Angeles County Emergency Medical Services Agency issued a directive that ambulance crews should ration supplemental oxygen, only administering it to patients whose oxygen saturation levels fall below 90%.
The situation is particularly grim in Los Angeles County, where one person is dying from COVID-19 every 10 minutes. The Los Angeles Times reported that the county’s four public hospitals are preparing to shift to a rationing system in which a central team of triage officers would decide which patients “get access to resources such as ventilators, respiratory therapists, and critical care nurses when they become too scarce to be provided to every patient.”
The pandemic crisis has exacerbated already stark health disparities in California’s most populous county. Latinx residents are now dying of COVID-19 at 2.5 times the rate of White residents. “The progress we’ve made over the summer has completely evaporated,” Barbara Ferrer, PhD, MPH, director of the LA County Department of Public Health, told the Los Angeles Times. “The gaps again have dramatically widened, particularly for Latinx residents compared to other groups.”
UK Mutation Migrates to California
Ever since the coronavirus variant B.1.1.7 was detected in the UK in December, California has identified dozens of those infections, including 26 in Southern California alone. This is very likely an undercount, because the US lacks a single system for sequencing coronavirus genomes. A patchwork of academic, state, and commercial labs is sequencing roughly 3,000 genomes a week nationwide, Carl Zimmer wrote in the New York Times.
The variant is estimated to be 50% to 70% more infectious than other versions of the virus, although it is not thought to be more deadly. However, as Zeynep Tufekci wrote in the Atlantic, “Given the stage in the pandemic we are at, a more transmissible variant is in some ways much more dangerous than a more severe variant. That’s because higher transmissibility subjects us to a more contagious virus spreading with exponential growth, whereas the risk from increased severity would have increased in a linear manner, affecting only those infected.”
The good news is that we know how to handle this variant — we just “need to do it better,” Kristian Andersen, PhD, professor of immunology and microbiology at Scripps Research, told CalMatters. This means ramping up vaccinations while doubling down on public health measures like mask wearing, hand washing, and physical distancing, he said.
What questions do you have about the COVID-19 vaccine rollout or the new virus variant? Email me.
Authors & Contributors






