When adequately supported and designed, high-quality primary care is a common good that provides better population health and more equitable outcomes, according to the National Academies of Sciences, Engineering, and Medicine (NASEM).
But primary care in the US has been under-resourced for decades, especially in Black, Indigenous, and other historically marginalized communities, resulting in a depleted workforce struggling to deliver care in a weakened infrastructure. The first National Primary Care Scorecard released in February underscores this reality and demonstrates that our current primary care policies are not adequately supporting the delivery of high-quality primary care.
Recognizing this, the federal government recently launched the Health and Human Services Initiative to Strengthen Primary Health Care, and 17 states are adopting legislation to increase investment in primary care. A new report sponsored by CHCF summarizes decades of research that demonstrate the link between primary care and improved health equity. In this report we argue that more needs to be done – and done differently – to rebuild the foundation of our health care system in an equitable way.
A Paradigm Shift
Our CHCF-sponsored report calls for new ways of thinking and acting as we work to strengthen primary care and ensure these efforts prioritize equity:
- Recognize high-quality primary care as a common good
- Embrace the diversity of primary care practice settings and invest resources according to need with the intentional goal of reducing health and social inequities
- Proactively apply principles of equity and justice to all decisions
- Build accountability for action
- Achieving such a paradigm shift is challenging from a policy perspective. What will policymakers and other decision-makers need to consider as they implement these policies?
Policy Principles
Primary care access, quality, and resources vary widely between communities. These disparities reflect decades of differential investment and fall most heavily on disadvantaged communities, including those at highest risk for health inequities, such as Black, American Indian, and Alaska Native populations. More investment in primary care is needed. Any future programs and investments must advance equity in primary care. Specific solutions will (and should) vary across states, but here are four overarching policy principles:
- Commit to immediate action and maintain a long-term perspective on returns. Primary care practices need assistance and more equitable payment models now. Our recent CHCF-sponsored report provides examples of primary care policy recommendations that could be acted on immediately to advance health equity in California and in other states. But successfully addressing long-term deficits in support for primary care and long-standing health inequities requires time, flexibility, and persistence. While evidence supports cost savings over time, expectations of short-term return on investment can perpetuate health care inequities and can undermine long-term commitments to increasing primary care spending and provider payments.
- Create stable, collaborative, sustainable processes for dialogue with primary care practices and communities about their needs. Investing resources according to the needs of diverse primary care practices in the context of their communities starts with prioritizing communities with the least access and availability of high-quality primary care. This must include asking community members, patients, and the practices in these places what they care about and what their priorities are. As a result, governments, payers, purchasers, and others need to find ways to work together to support equity-driven community and practice-level needs assessments (not just one time, but repeatedly) and use the identified priorities to help guide investments in primary care and in efforts to reduce inequities in access, quality of care, and outcomes.
- Think creatively about investments and funding and use multiple approaches to address different needs. Primary care practices in historically marginalized and under-resourced communities need more investments and support to move toward and succeed within flexible, equitable payment models that are value-based. Using small-area deprivation measures — measures based on health in neighborhoods such as the Area Deprivation Index (ADI) or the Social Deprivation Index — in addition to patient-specific characteristics, social needs, and health conditions already included in risk adjustment, policymakers and payers can increase payments and investments for practices that serve patients and communities that face higher levels of health and social inequities. Practices also need investments and support to connect effectively with community-based organizations that can help address patients’ health-related social needs such as housing instability, food insecurity, and transportation. In addition, investments in health workforce development are critical so that practices can hire primary care team members from the local community and provide meaningful career advancement opportunities.
- Make all partners accountable for progress, not just primary care practices. Prioritizing equity in primary care is an “all hands-on deck” activity that will require stronger governance and accountability mechanisms that encourage participation and oversight from patients (including people with lived experience dealing with health and social inequities), communities and community-based organizations, practices, public health systems, payers, policymakers, and others. This means that all parties – not just primary care practices – are aligned and accountable for advancing primary care’s essential role in advancing health equity. Massachusetts Health Quality Partners led the way earlier this year by publishing a dashboard of primary care metrics to drive policy initiatives and target resources in the state; other states should follow suit.
Applying These Principles
To forge a path toward health equity, innovative primary care policies and investments are needed in communities across the nation, and a one-size-fits-all approach will not suffice. Strengthening primary care in a way that assures equity for patients, communities, and health care workers will require a radical reorientation of payment and policy.
We encourage decision-makers to use new policy levers, or use old levers in new ways, asking these questions:
- Could tax policy be used to provide relief for struggling independent practices, or provide incentives for practices and health systems to partner with community-based organizations to address health inequities?
- What types of new partnerships are possible across levels of government, including municipalities, counties, states, and the federal government?
- Can we leverage public funds and regulations (e.g., through state Medicaid agencies) to align primary care capacity, systems, and improvement efforts with broader place-based public health and community-led efforts to advance population health and health equity?
In addition, infrastructure investments can take many different forms. Two possibilities to consider are:
- Funding a federal primary care extension service – primary care extension agents can facilitate community engagement with primary care and public health and collaborate with primary care practices (of all types) in needs assessment, service improvement, and accountability
- Funding Community-Based Organization Networks, hubs that can support contracting between community organizations and healthcare providers
As a common good, primary care should be promoted, protected, and monitored by responsible public policy and supported by private-sector action. Progress is possible. And the time is now.
This article was first published by the Milbank Memorial Fund and is reprinted with permission.
Authors & Contributors

Diane Rittenhouse
Diane Rittenhouse, MD, MPH, is a senior fellow at Mathematica and a professor of family medicine and health policy at University of California, San Francisco. She is nationally recognized for her research on innovations in primary care organization, delivery, finance and workforce — and her ability to translate this research into policy. She has led many studies that have contributed to health care reform discussions.
She was principal investigator for the evaluation of federal efforts to restore, expand, and improve primary care services in greater New Orleans following Hurricane Katrina and co-investigator on multiple large national studies of physician practices. She is principal investigator for the transitional program office to expand graduate medical education in California. She is also principal investigator for a qualitative study of high-performing physician-owned private practices.
Rittenhouse has published in the Journal of the American Medical Association and the New England Journal of Medicine and has been cited in The New York Times, the Wall Street Journal, the Los Angeles Times, and USA Today.
She received her MD from the University of California, Davis, and her MPH with an emphasis in health policy and management from the UC-Berkeley. Before her medical training, she worked for the California Statewide Office of Health Planning and Development and for the deputy assistant secretary for health in Washington, DC.

Janice L. Genevro
Janice L. Genevro, PhD., MSW has worked for many years to improve health care services, health system-community collaboration, and health. Her work with colleagues at the US Agency for Healthcare Research and Quality and later at Mathematica focused on primary care practice improvement.
She is currently an independent consultant.


Rishi Manchanda
Rishi Manchanda, MD, MPH is CEO at HealthBegins, a national firm that helps Medicaid-serving executives and teams meet growing state and federal requirements for health equity and social needs, exceed performance goals, and achieve long-term impact for people harmed by societal practices. He has advanced this mission throughout his career as a primary care physician, executive, and public health champion.
Manchanda served as founding director of social medicine for community health centers in south central Los Angeles, as the first lead physician for veterans experiencing homelessness at Greater Los Angeles Veterans Affairs health services, and as inaugural chief medical officer for a self-insured employer with a large rural agricultural workforce.
In his book The Upstream Doctors and in a TED Talk, he introduced a new model of health care professionals known as “Upstreamists.” They focus on improving outcomes by addressing social and structural drivers of health equity, including patients’ social needs, community-level social determinants of health, and structural determinants of health equity such as structural racism.

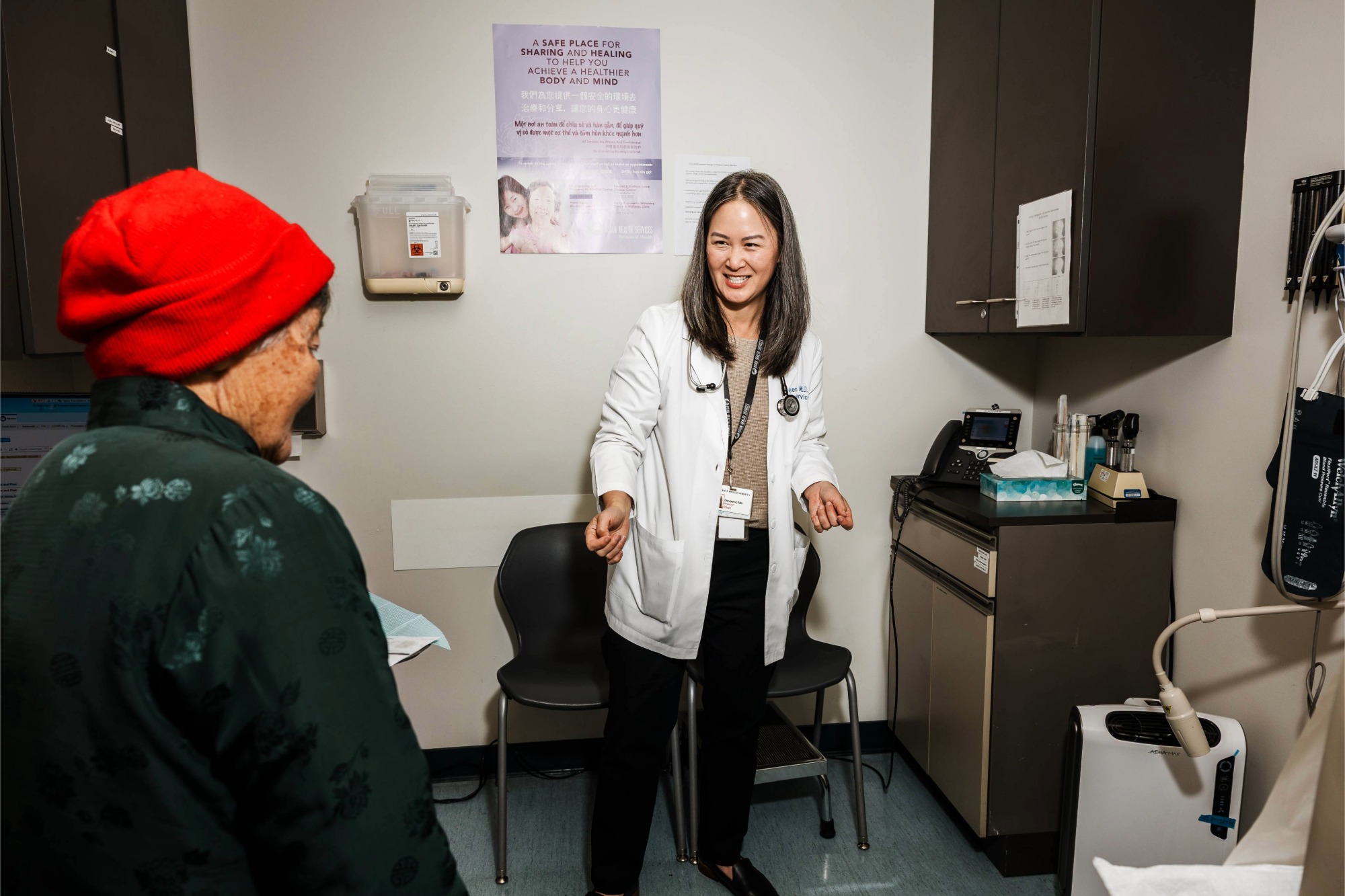
Jessica Brandi Lifland
Jessica Brandi Lifland is a freelance photographer, instructor of journalism at City College of San Francisco, and mother. Her work with publications and nonprofits such as Operation Smile, Tostan, and the California Health Care Foundation has taken her all over the world, including West Africa, the Middle East, Kosovo, Burma, Haiti, and South America.
For two decades she has been photographing the National Cowboy Poetry Gathering and has been working on a long-term project documenting the lives of the cowboy poets of the American West in affiliation with the Western Folklife Center. She plans to make her project into a book.