California led the nation in health care reform by enabling millions to obtain health insurance through the Affordable Care Act. This year, by expanding Medi-Cal to all Californians with low incomes, regardless of immigration status, our state will achieve another milestone: historically low numbers of residents lacking health insurance.
Having an insurance card, unfortunately, doesn’t guarantee access to a primary care team that knows you, your family, or your community. Absent such relationships, many get lost in or ignored by the system, or don’t trust it — as shown during the COVID-19 pandemic. California’s next challenge is to resolve the mismatch between coverage and quality care by making sure all of us have access to primary care.
To address this, Covered California and the California Public Employees’ Retirement System are working with other health care leaders statewide to strengthen primary care.
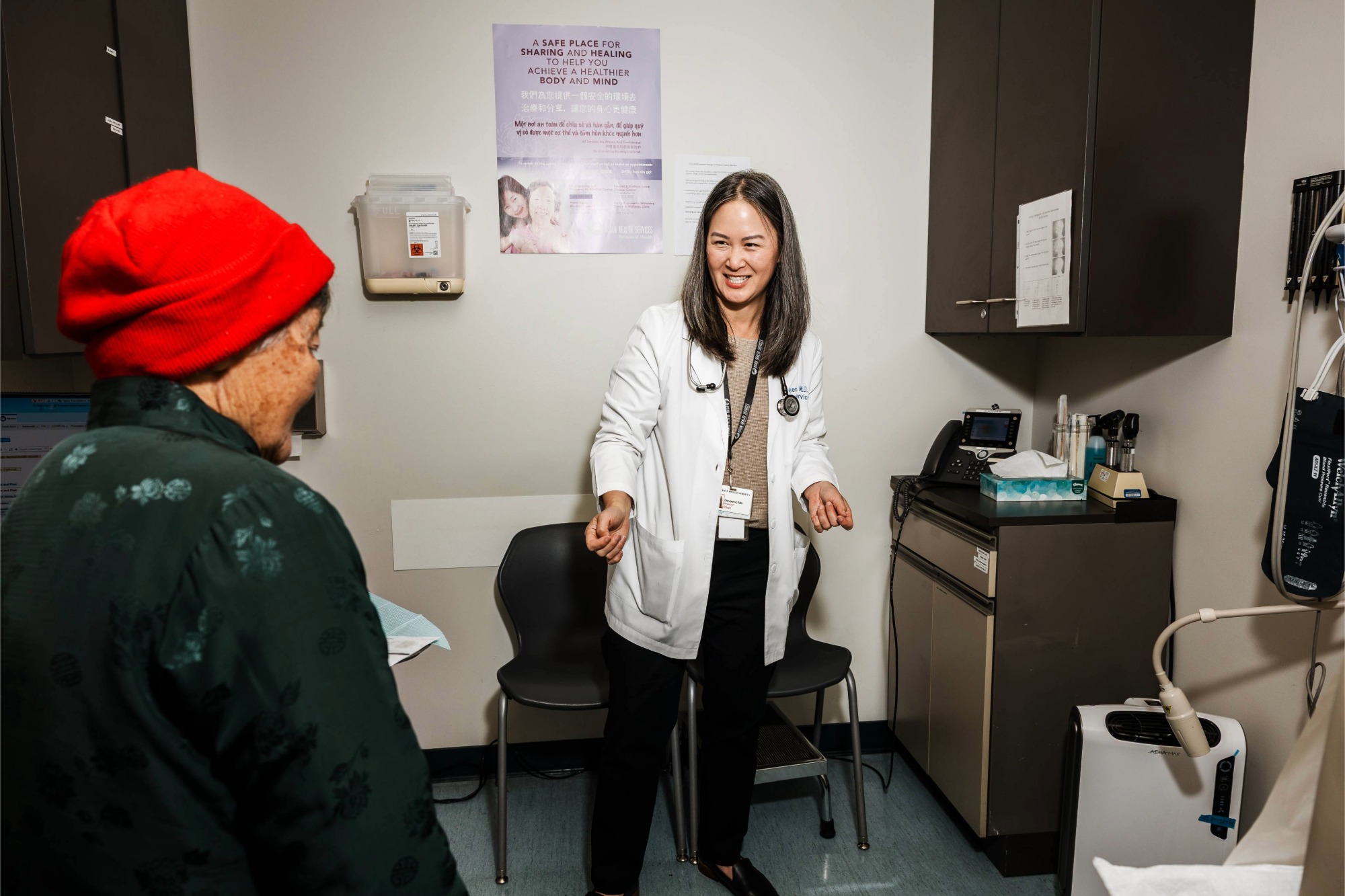
By reorienting health care back to patients and their relationship with primary care providers and teams — including physicians, nurse practitioners, physician assistants, community health workers, and behavioral health staff — we can build a health care system that’s better at keeping us healthy and rooted in our communities.
Access to high-quality primary care is essential. Primary care teams help patients and families address physical and behavioral health needs — from prevention to new sicknesses to managing chronic disease to end-of-life care. They help patients overcome social stressors that impact health, such as violence or food insecurity, and navigate the health care system by coordinating testing and specialist care when needed. Most importantly, they become a trusted advocate for patient health and well-being.
A first-of-its-kind study of primary care spending in California’s commercial health insurance market finds organizations that invest a higher proportion of spending in primary care deliver better care. Encompassing 80% of California’s commercially insured adults, the study found the percentage of primary care spending among health maintenance organizations, preferred provider organizations, and exclusive provider organizations varied from 4.9% to 11.4%.
The study delved deeper into primary care spending among 180 provider organizations serving 8.5 million people enrolled in health management organizations — almost half of California’s commercially insured adults. A higher percentage of primary care spending was associated with better care quality and patient experience, fewer hospital and emergency room visits, and lower cost of care.
The study’s findings on variation in the level of investment reveal that many Californians may be missing out on primary care services that help them stay healthy. It suggests that increasing primary care investment could save an estimated $2.4 billion annually in care costs and prevent 89,000 emergency room visits among Californians enrolled in commercial health maintenance organizations.
A recent poll found that access to primary care also is a matter of health equity. Insured Californians with a primary care provider, compared to those without, report fewer health care access, language, and distance barriers. They also are less likely to report negative experiences with health care providers, such as being talked down to or not being listened to. Insured Latinos were the least likely to report having a primary care provider compared to other insured Californians.
As we know, you get what you pay for. That’s why our organizations are raising the bar for primary care investment among health plans we contract with to provide health insurance for more than three million Californians.
Starting next year, CalPERS will require preferred provider organizations to match members with primary care providers to improve care quality. Covered California will require health plans to measure and report primary care spending (PDF).
Ultimately, strengthening primary care benefits everyone. It puts patients back at the center of care. It ensures medical professionals interact with the patients who need them most when they need them. It helps keep care costs affordable.
Above all, it makes health care more accessible and responsive.
This article was first published by CalMatters on April 29, 2022.
Authors & Contributors

Alice Hm Chen
Dr. Alice Hm Chen is chief medical officer at Covered California, the state’s health insurance marketplace, which actively works to ensure that Californians can find affordable, high quality coverage. In this role she is responsible for health care strategy focused on quality, equity, and delivery system transformation with the goal of improving access and outcomes for all Californians.
Dr. Chen previously served as deputy secretary for policy and planning and chief of clinical affairs for the California Health and Human Services Agency. She led many of the Agency’s signature health policy initiatives on affordability and access, and played a leadership role in the state’s response to the COVID-19 pandemic in the areas of strategic reopening, hospital surge planning, equity, data analytics and therapeutics.
A graduate of Yale University, Stanford University Medical School, and the Harvard School of Public Health, Dr. Chen’s training includes a primary care internal medicine residency and chief residency at Brigham and Women’s Hospital. She is an alumna of the Commonwealth Fund Harvard University Fellowship in Minority Health Policy, the Soros Physician Advocacy Fellowship, the California Health Care Foundation Leadership Program, and the Aspen Institute’s Health Innovators Fellowship. Proficient in Mandarin and Spanish, she maintains an active primary care practice at Zuckerberg San Francisco General Hospital and holds an appointment as clinical professor of medicine at UCSF.

Julia Logan
Julia Logan, MD, MPH is chief medical officer at the California Public Employees’ Retirement System. She joined CalPERS in May 2019. Dr. Logan leads the clinical policy program as well as CalPERS COVID-19 response efforts. Before CalPERS, she served as chief quality officer and associate medical director for the California Department of Health Care Services. She is a practicing physician, volunteering at a local community clinic to treat patients with all types of medical conditions. Dr. Logan graduated from Drexel University College of Medicine in Philadelphia.