View the Report
Jump to All Downloads & LinksTreatment and prevention of chronic illness threatens to overwhelm California’s health care safety net — the provider and payer organizations that serve people with low incomes. Long stressed by workforce shortages, the safety net is under increasing strain due to the rising prevalence of chronic conditions such as heart disease and diabetes in the patient population.
Remote patient monitoring is a type of telehealth that involves the secure transfer of personal health and medical data to a provider for remote monitoring, care, and support.
Encouraged by positive experiences with telehealth modalities during the COVID-19 pandemic, providers and payers are interested in additional ways to use technology for greater efficiency and access, including to facilitate chronic condition care and prevention.
To do so, some providers across the health care spectrum have incorporated remote patient monitoring (RPM) into their workflows. RPM is a type of telehealth that involves the secure transfer of personal health and medical data to a provider for remote monitoring, care, and support. Although not yet widely used among California’s safety-net providers — in part because of current Medicaid reimbursement policy — RPM offers potential for mitigating access barriers and facilitating care management for patients who have chronic conditions or who have warning signs of such illnesses.
Providers see the potential for RPM to improve connections with patients outside clinic walls, integrate services across the continuum of care, maximize workforce efficiency, expand access to care, and reduce health inequities.
This report includes a landscape scan of some of the available tools geared to chronic condition management. The research was done between November 2020 and February 2021 in an extremely fast-evolving marketplace, so the information shown is not complete. The report addresses several questions:
- What problems can RPM help solve?
- What do providers want and need from RPM?
- What are patients’ needs and perspectives?
- How is RPM currently reimbursed in Medicaid and Medicare?
- What should providers know about starting or scaling up a program?
- What is the outlook for RPM in the safety net?
- What is the landscape of emerging companies focused on RPM?
Rates of avoidable hospitalizations in California are highest among Medi-Cal beneficiaries; nearly 700 hospitalizations per 100,000 people are potentially preventable through effective chronic care management and access to primary care. Such numbers point to unnecessary suffering for people with chronic conditions as well as unnecessary expense for the safety-net system. Providers, payers, and all Californians have an interest in leveraging technologies that can assist in the management of chronic illnesses.
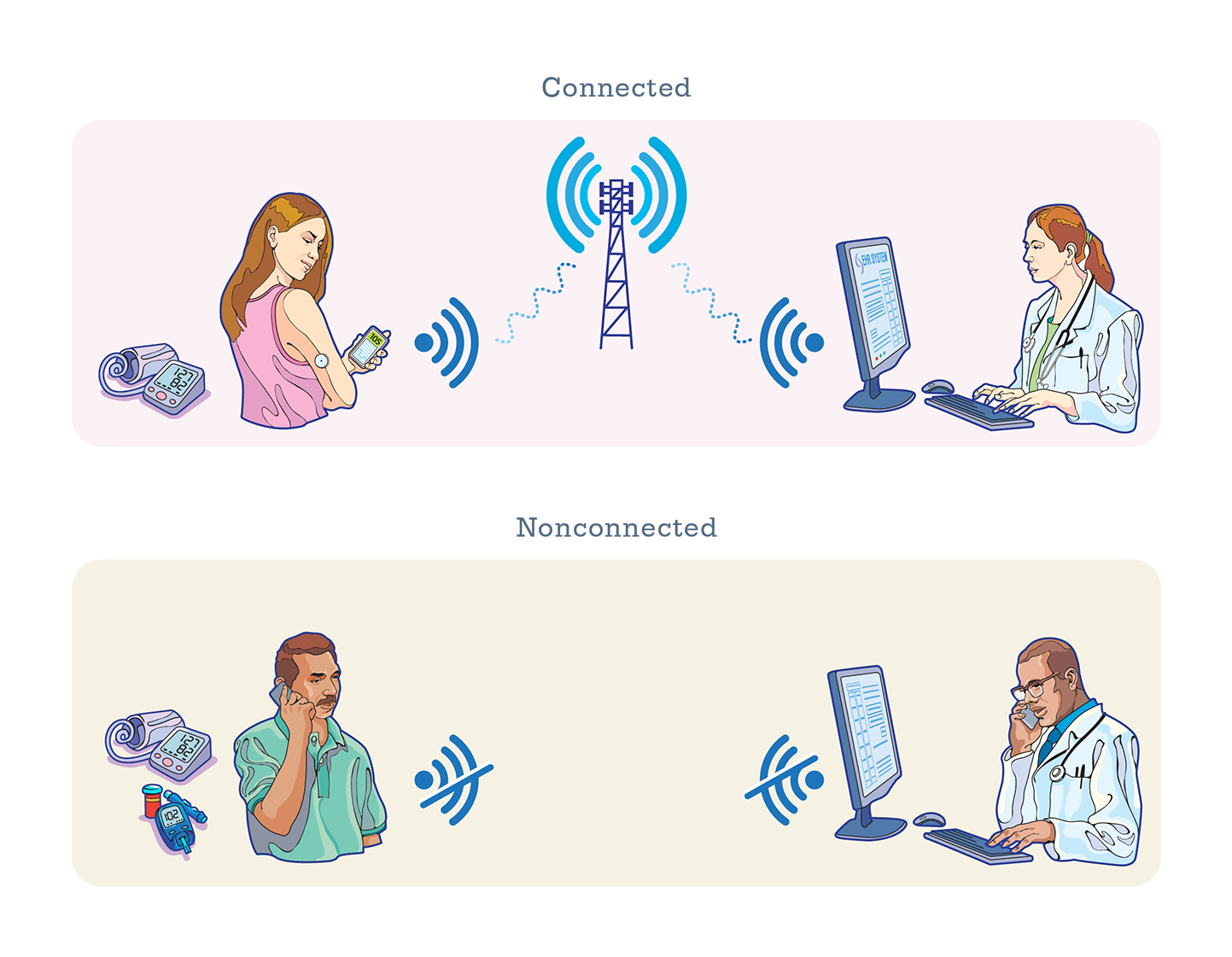
Connected Versus Nonconnected Devices
Safety-net providers often weigh the pros and cons of using “connected” or “nonconnected” devices:
- Connected RPM devices automatically transmit data through the internet or a cell phone into an analytics platform that providers and patients use to view the data and manage care. Such connected devices lessen the number of manual steps required for patients and providers to collect and deliver data. However, the connected devices are more expensive than nonconnected devices — in some cases twice as expensive — with integration into the provider’s EHR system being yet another expense.
- Nonconnected devices require patients to manually report health measures such as blood sugar and blood pressure through a patient web portal, by text message, or during a visit with their provider. Many clinics choose such low-tech RPM methods because of cost factors and limited access to internet or cellular data. However, these solutions require the provider to develop workflows to capture data and may present additional challenges if readings are not accurately reported by patients. Providers and other stakeholders emphasized the need for RPM program operations and workflows to be thoroughly considered before a technology is selected. Cindy Keltner of the California Primary Care Association noted, “Our clinics are very concerned with the workflow implications in terms of monitoring, managing, and acting on data as it streams in electronically.”
Figure 1 illustrates the difference between a connected and nonconnected device for remote patient monitoring.
What Is the Outlook for RPM in the Safety Net?
The limited research that exists indicates that RPM programs can deliver strong clinical outcomes when applied to safety-net populations.
The most valuable information, experts said, would come from rigorous, large-scale evaluations of the clinical impact and cost-effectiveness of RPM programs, conducted by provider organizations with research funding. Such a fiscal impact analysis would support changes in coverage and payment that would in turn facilitate broader market adoption.
Authors & Contributors
Andrew Broderick, MBA
Andrew Broderick is research program director at the Public Health Institute (PHI).
Valerie Steinmetz, MPH
Valerie Steinmetz is program director at PHI.
Michael Benzinou, PhD
Michael Benzinou is founder of Elements Innovation.
Sarah Carroll, MPH
Sarah Carroll is senior director at the Center for Care Transformation, AVIA.
Hanna Helms
Hanna Helms is senior manager at the Center for Care Transformation, AVIA.



