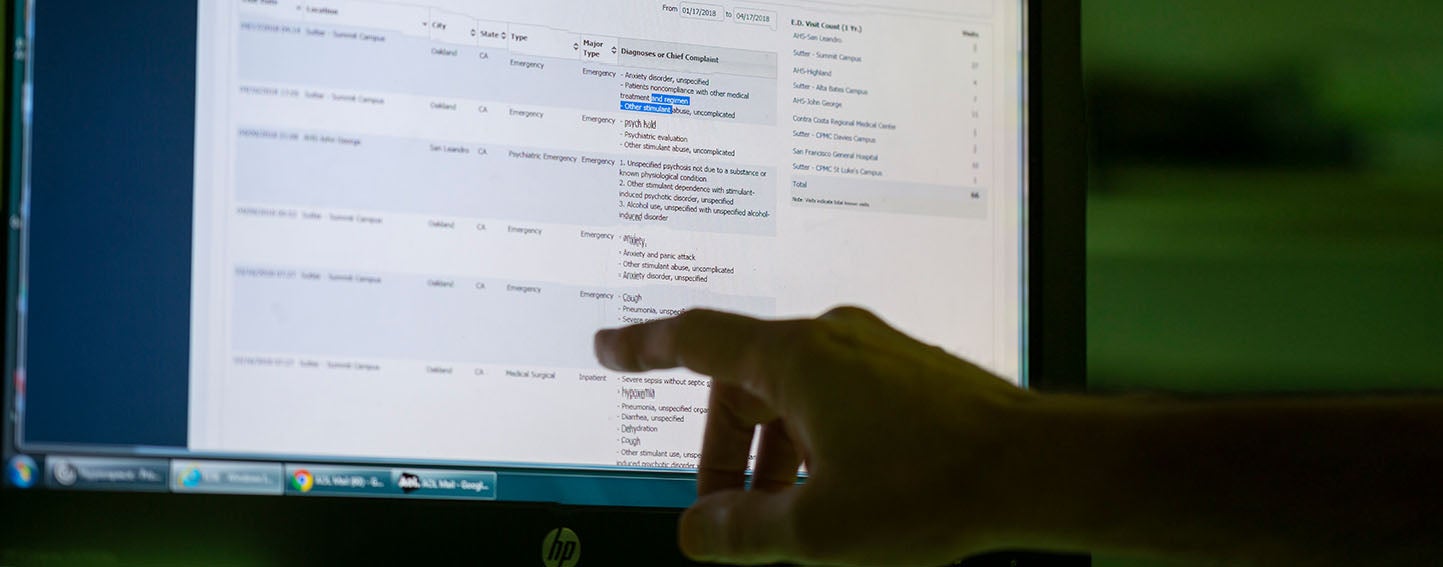
Electronic health records (EHRs) — repositories of patient medical histories, billing codes, and other crucial information — play a vital role in the operations of 90% of California’s community health centers (CHCs). Increasingly, this role has expanded to population health management, tracking social determinants of health, and enabling better care coordination for patients with complex needs, among other things.
This evolution is driving some clinic leaders to consider whether their current EHR system can keep up with growing demands. A recent survey of outpatient providers found more than one in four are actively considering switching EHR platforms. Numerous CHC leaders are reassessing their EHRs and have a wide range of reasons for considering a switch. Not every situation was alike, so each organization took its own unique decisionmaking journey. One thing they all shared, however, was the belief that having a guide to help them weigh options and forge the path forward would have been enormously useful.
To Switch or Not to Switch: A Guide for Community Clinics Considering Changing EHRs provides that help. The guide’s author, Walter Sujansky, MD, a consultant on EHR analysis and design, interviewed California safety-net leaders and EHR vendors. For many, the question of whether to change EHRs is a priority — and there is no right answer to it, he found. But interviewees did identify similar goals for updating systems:
- Improving interoperability with specialists and hospitals that use a different EHR
- Reducing complexity and cost by outsourcing day-to-day EHR management
- Responding to clinic staff members who prefer a different EHR product
- Sharing a common EHR across a CHC consortium, especially if its members participate in alternative payment and risk-sharing programs with payers
The guide offers a thorough and balanced decisionmaking process that applies to any clinic. Sujansky outlines key steps and includes helpful questions to ask at each waypoint.

The Voice of Experience
Recently I spoke about the EHR updating process with Sabra Matovsky, MBA, CEO of the San Francisco Community Clinic Consortium and former executive vice president of Integrated Health Partners, a network of 11 health centers in the San Diego area. Here is our conversation, lightly edited for clarity.
Q: What motivates health centers to consider switching?
A: As we think about taking care of our managed care population in a more coordinated and data-informed way, the tools we use become a critical consideration. We can no longer look at an EHR merely as a tool to manage care patient-by-patient. As a result, CHC leaders are asking themselves, “Is our EHR system supporting us in offering the best care we possibly can to our patient population?”
Q: You’ve led two major organizations that considered EHR switches. What would you tell someone considering this for their operation?
A: Take a good look at all your options for a switch. People can have a preconceived idea of what they want. The existing solutions may only be able to meet a subset of those needs. Because of this, it can be particularly helpful to have an impartial person who will support you in evaluating and vetting vendors. And finally, while you may be able to identify why a switch would be beneficial, it’s important to carefully weigh the financial and operational impact and consider how, if, and when you can realistically resource the change.
Q: What did you learn about the process of planning a switch?
A: Don’t underestimate the challenges of group decisionmaking, either within the context of your own health center — with the staff and board — or if you are deciding as a network of clinics. People may have a big investment in their current EHR and can have very different ideas about what they need. Allow time to build consensus. If you are a part of a network of clinics, it may make more sense to go with a few early adopters rather than try to bring everyone along at the same time. Once a critical mass gets behind a single system, it presents an opportunity.
Q: What other advice do you have for those who do decide to move forward?
A: Going through the process haphazardly is not going to achieve results. You need to have discipline through implementation. You should also set up systems and allocate the needed resources to enable you to consistently improve and modify the system as your needs evolve. Otherwise, you may end up on another EHR shopping trip in a few years.
Authors & Contributors






