
For providers in the safety net, tasks as simple as keeping a patient’s home address up to date or sharing a patient’s health record with another entity can be especially difficult. The reasons are many, but the effect is the same: care is delivered more slowly, at lower quality, or less accessibly. The California Health Care Foundation Innovation Fund is part of a growing national movement working to harness technology to remove these kinds of barriers for Medicaid plans and providers. The Innovation Fund focuses on technological solutions with the potential to improve access and health outcomes for Californians with low incomes. The innovation opportunity in California and across the nation is huge — one in five Americans is enrolled in a state Medicaid program.
One technology company CHCF supports is RubiconMD, which is tackling a seemingly simple but frustrating challenge facing Medicaid providers: referring patients to a specialist. Wait times are long within many specialties and geographic areas, especially for Medi-Cal beneficiaries. They are more than twice as likely as privately insured people to report difficulty accessing specialty care. At the same time, studies show that a significant portion of specialist visits are unnecessary. RubiconMD addresses these problems simultaneously by enabling primary care providers to get advice from specialists electronically. This solution, also known as an electronic consult, or eConsult, helps patients avoid the delays and frustrations that follow primary care physicians’ referrals. It also lets health systems make more efficient use of the limited time of overburdened specialists.
Many entrepreneurs are interested in following RubiconMD’s lead, but they frequently express common concerns about leaping into the Medicaid world, where state-level differences are significant and populations diverse. That can make it hard to replicate successes in new markets.
Out of a belief that these concerns may be overblown, CHCF partnered with Village Capital and Speire Healthcare Strategies to launch Primed, a series of four statewide roundtables that brought together payers, providers, state Medicaid officials, investors, and entrepreneurs to share their innovation successes and challenges.
Medicaid Road Trip
The Primed events were held in Colorado, Massachusetts, Tennessee, and Washington, DC. When asked to identify the areas within Medicaid where technology-enabled innovation is needed most, attendees at all four roundtables prioritized the same four essential challenges (see our complete infographic on these challenges at the link below).
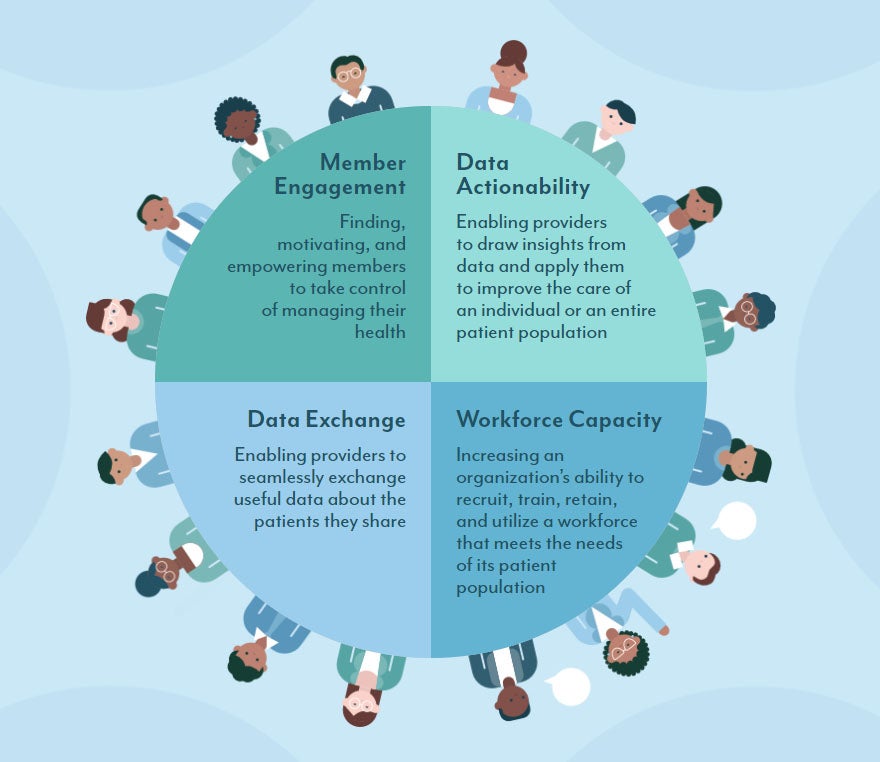
This interstate consensus surprised many participants and reaffirmed a basic truth: If you’re offering a real solution to one of these pressing problems, Medicaid is a $550 billion market with immense potential for scale and impact.
Virtual Care on the Rise
RubiconMD executives wanted to validate the effectiveness of electronic consults (eConsults) for improving access to specialty care in the safety net, so they participated in an evaluation in a large public health system. This type of evaluation is a standard requirement of companies supported by CHCF’s Innovation Fund. It helps newer companies prove their value to Medicaid programs. Three years after the health system adopted eConsults, wait times for specialists had decreased by an average of 17%, and one in four eConsults was resolved without requiring an in-person specialist visit. An evaluation conducted in a different safety-net system also demonstrated that many primary care providers believe eConsults improved the quality of care they deliver to their patients.
Another technology company poised to serve the Medicaid population is New York–based AbleTo, which provides virtual behavioral health care to people with depression, anxiety, or stress associated with comorbid medical conditions and life events. The program identifies members living with undiagnosed mental health conditions and connects them to licensed providers who deliver therapy and coaching from remote locations. In an evaluation of AbleTo’s program for patients with chronic pain (PDF), participants experienced meaningful reductions in the severity of depression, anxiety, and stress symptoms. These types of virtual care models enable more productivity from the same number of providers while helping patients overcome great distances or limited access to transportation to get care from therapists or coaches.
When CHCF launched the Innovation Fund in 2010, few individuals were starting or investing in technology companies focused on Medicaid. That began to change with the 2014 implementation of the Affordable Care Act as millions signed up for Medicaid services. Entrepreneurs and investors wanted to meet the needs of this growing population. But they quickly learned those needs can be complex — many Medicaid beneficiaries have multiple health conditions and also experience numerous barriers to receiving care.
Looking Ahead
Fortunately, in the last few years more organizations have emerged to help overcome these challenges by harnessing significant capital and in the process attracting national attention. HealthTech4Medicaid formed a coalition of more than 40 CEOs, whose tech companies collectively represent more than $1 billion in venture capital backing, advocating for innovation in Medicaid. The Medicaid Transformation Project, led by AVIA, an innovation network and health care consulting firm, and former Centers for Medicare & Medicaid Services administrator Andy Slavitt, is engaging 28 major health systems to improve outcomes for Medicaid beneficiaries receiving maternity care, behavioral health services, and other categories of care. And venture firms like Town Hall Ventures and accelerator programs like Adaptation Health are helping promising companies attract capital and serve greater numbers of Medicaid plans and providers.
We hope the results of CHCF’s roundtable series offer a road map for how to sustain this growing momentum and translate it into meaningful care improvements for Medicaid beneficiaries.
To learn more about solutions already at work in Medicaid, check out our Primed infographic.
Authors & Contributors




