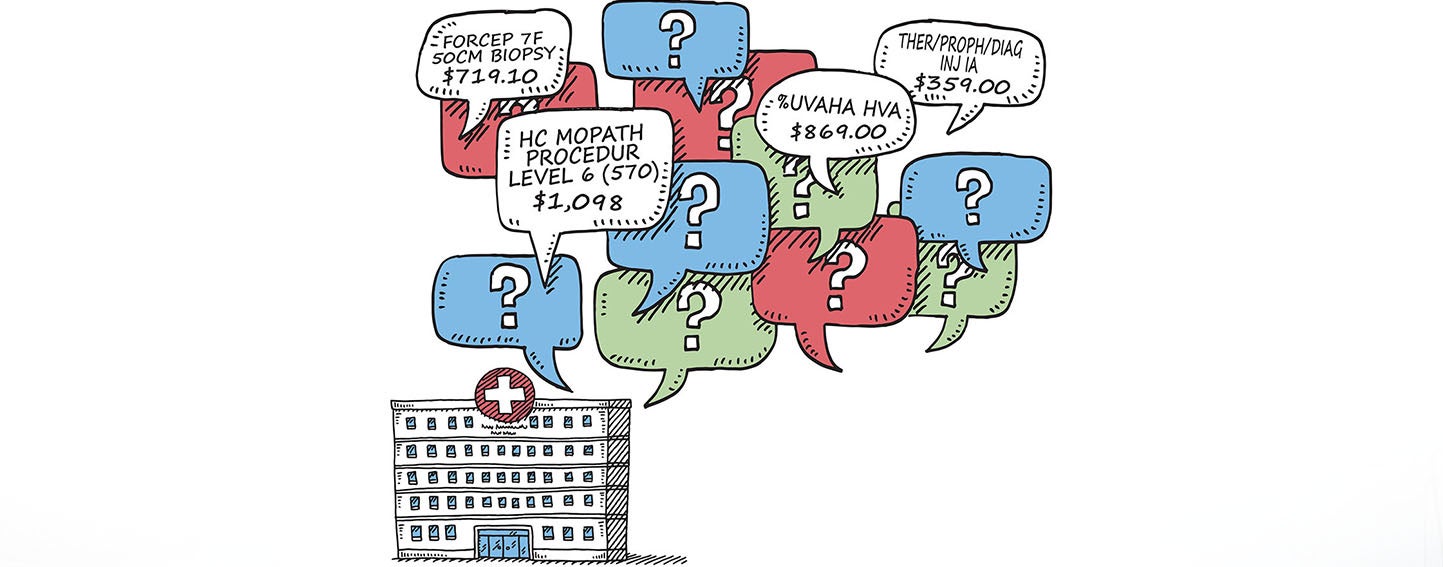
If knowledge is power, patients across the country got stronger on January 1, when a new national health care transparency policy took effect. All hospitals must now post their price lists online. In theory, this information should empower consumers to shop around for health care services. But some critics have dismissed the lists, called chargemasters, as meaningless and incomprehensible.

Kaiser Health News describes chargemasters as “massive compendiums of the prices set by each hospital for every service or drug a patient might encounter.” The adjective “massive” is no exaggeration — the UCSF Medical Center chargemaster weighs in at more than 88,000 rows. Each row lists the price for a specific service, for example “GRAFT VASC AORTIC ARCH ANTE-FLO 22 MM 732022/8” for $4,490.
In the New York Times, Robert Pear likens each chargemaster price to the sticker price for a car. This is problematic, he writes, because “it is as if the car dealers were disclosing the price for each auto part, without revealing the charge for the vehicle as a whole.” So the idea that a patient would find the sticker price of “GRAFT VASC AORTIC ARCH ANTE-FLO 22 MM 732022/8” to be helpful information about, say, the cost of a heart valve replacement surgery is preposterous.
Furthermore, as Sarah Kliff explains in Vox, chargemasters lay out the list prices that hospitals charge for services, not the prices insurers actually pay. “Some research has found that the actual prices insurers and patients pay bear little relationship to the published charges,” she writes. For example, the Economist alludes to an analysis of payments for uncomplicated births in California that “found that discounted prices paid by insurers were, on average, 37% of hospitals’ list prices.”
A Small Step Toward Transparency for Consumers
The new rule requires hospitals to post their chargemasters online in a format that can be easily processed by a computer. In a speech at the Commonwealth Club in July 2018, Centers for Medicare & Medicaid Services Administrator Seema Verma hailed the requirement as “a small step towards providing our beneficiaries with price transparency.”
But what’s a patient to do with the complicated information provided by hospitals? Martin Gaynor, professor of economics and health policy at Carnegie Mellon University, told Kliff, “I would say [the answer is] nothing. I don’t think this is useful information.” Caitlin Donovan, director of outreach and public affairs at the National Patient Advocate Foundation, told Marketwatch, “I doubt most hospitals went through the process to make these as consumer-friendly as possible.”
There are exceptions, especially in California. Since 2004, California has required hospitals to disclose their chargemasters; two years later, the state added a requirement for reporting a list of charges for 25 common outpatient procedures. Over time, some hospitals in California have opted to modify their reporting to become more patient-friendly. For example, El Camino Hospital in Silicon Valley offers free, confidential estimates for services performed at the hospital, and provides a self-service price estimator tool on its website.
All this is to say that while simply disclosing chargemasters is no panacea for patients’ health care cost woes, it is a step in the right direction. In a letter to the New York Times, Sharrie McIntosh, the vice president for programs at the New York State Health Foundation, suggests following the reporting requirement with “uniform standards for how prices are reported across hospitals so that patients are comparing apples to apples when comparison shopping.”
Kristof Stremikis, director of CHCF’s Market Analysis and Insight team, said disclosing chargemaster prices could help patients in the long run. “This is machine-readable data that could facilitate bundling individual charge codes into larger episodes that patients are more familiar with,” he said. “The data and trends revealed by annual disclosure will yield more insights than one might expect.”
Look for a post from Stremikis on this topic soon in The CHCF Blog.
Have you explored any chargemaster data since the new rule went into effect? Tell me what you found — email me.
Authors & Contributors





