|
Getting your Trinity Audio player ready…
|
More than 20 years ago, I stepped into a clinic in San Francisco that provided health care to people experiencing homelessness. I was a new medical resident, wide-eyed and eager to use my training to help society’s most marginalized people, but I had little understanding of how to accomplish that goal.
The clinic’s patients became my teachers. They humbled me with their stories of unimaginable suffering and astonishing strength. And they taught me a critical lesson: To improve people’s health, we must address their social needs, including housing. That realization changed the trajectory of my career. Today, I have spent most of my professional life working to advance our health systems’ care of people who are unhoused.
Key to this effort has been building partnerships between the health care and housing sectors. I spent 14 years as a primary care doctor and hospitalist at a large, urban public hospital as well as a decade leading a medical respite facility. Later, I served as a medical director attending to population health strategies for a Medi-Cal managed care plan in Alameda County. In both capacities, I worked with county agencies, community partners, and advocates to develop strategies to meet the needs of people with complex situations, including people experiencing homelessness. Despite these efforts, true collaborations and partnerships with housing and homeless services organizations during those years could not be brought to scale.
Today, as leader of the California Health Care Foundation’s efforts to improve care for people with complex behavioral health and medical conditions, I am elated to report that this arena is seeing a significant change in perspective. After years of slow progress and unsuccessful attempts to create a more seamless system of care for people experiencing homelessness, I believe that genuine transformation is now underway.
Several colliding forces have made this moment possible, including widespread acceptance among service providers and policymakers that housing and health are connected; California’s allocation of Medi-Cal funding to provide housing services and supports for people who are experiencing or at risk of homelessness; and the COVID-19 pandemic’s stark demonstration that homelessness is a public health crisis.
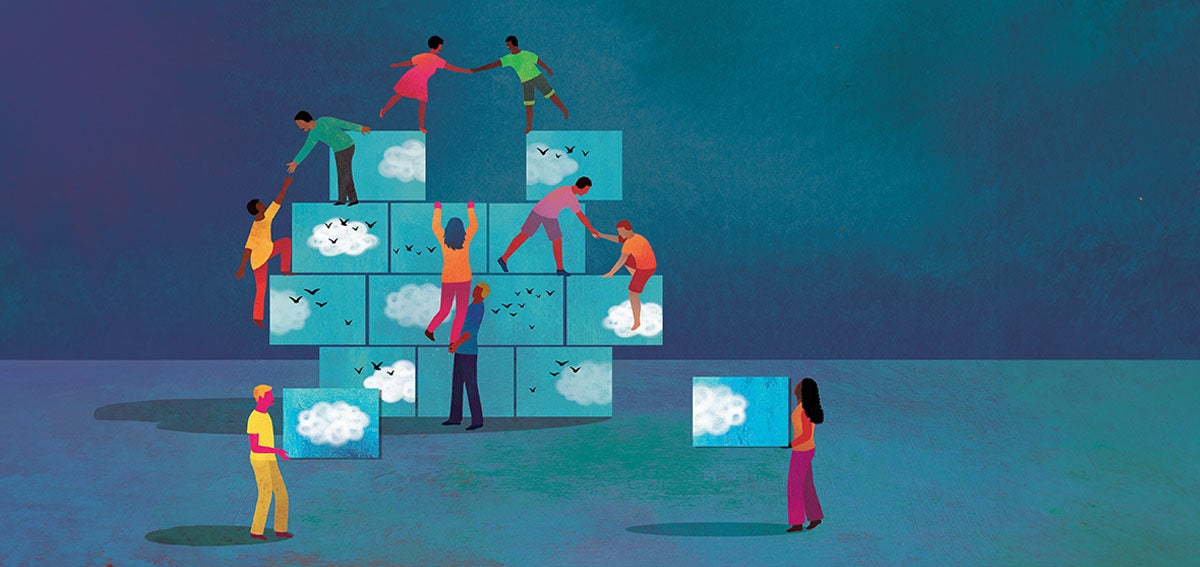
As a result, silos have broken down and unprecedented collaboration between the health care and homeless service fields has emerged. This is a seminal moment, and CHCF and our partners are working to accelerate it.
Community Effort Tackles a ‘Disconnect’
I first became conscious of the fragmentation within and between our medical and housing services sectors while working at San Francisco General Hospital (now the Zuckerberg San Francisco General Hospital). Like many physicians treating people experiencing homelessness, I endured the moral injury of having to discharge patients back into the streets after investing time, energy, and resources to stabilize their health conditions. Invariably, patients’ living situations undermined their abilities to recover and heal, and many returned to the hospital sicker than before. These systems failures not only felt inhumane and unethical, but also made no financial sense.
In the mid-2000s, I joined a community effort to tackle this disconnect. Stakeholders from across San Francisco came together to create our county’s first medical respite facility for unhoused patients — a safe place for patients to recover after being released from the hospital. I was the inaugural medical director, and I learned tremendous amounts from working with a multidisciplinary, cross-sector team to shape the program.
But launching the respite facility only addressed part of the problem, as patients still needed a place to go after discharge. We wanted to place them in permanent housing that could support their needs and prevent them from getting sick again, but executing such a plan proved extremely difficult.
First, the available housing supply was insufficient then much as it is today. Second, the homeless response and health care systems operated independently and had different definitions, policies, and incentives regarding prioritizing the needs of unhoused people with health problems. This lack of alignment and shared language created tension and an atmosphere of frustration between the two service sectors. The result was a disjointed, ineffective approach to moving the needle on homelessness.
Homeless — A Critical Social Driver of Health Status
That’s why I’m so excited by the pace of change over the past few years. I’ve always believed that homelessness is an “all hands on deck” issue. Now, the level of cooperation happening in California is beginning to reflect that. The changes are many. They include:
1. A shared understanding that homelessness is a critical social driver of health status. I used to spend much of my time making the case for the inextricable link between health and housing. I don’t have to explain that relationship anymore. Thanks to critical research on the subject, including last year’s statewide study on homelessness, providers of health care and homeless services now share this understanding. Health care alone cannot solve the homelessness crisis, but most people today recognize that it has an important role to play.
2. More available Medicaid dollars. With federal approval, California and at least 18 other states are funneling Medicaid money toward housing supports. California’s effort is among the most ambitious, with Medi-Cal channeling much of a $12 billion investment toward helping people experiencing homelessness find, pay for, and keep housing. Medi-Cal dollars are also financing an expansion of medical respite care. These changes are central to the state’s redesign of Medi-Cal, the California Advancing and Innovating Medi-Cal (CalAIM) initiative. The influx of Medicaid funding directly incentivizes collaboration between the health care and homeless service sectors, and Medi-Cal MCPs are now contracting with their local homeless service organizations to provide housing navigation, care coordination, other supports. Changes in Medicaid billing have also encouraged the growth of innovative health care delivery models, such as street medicine and mobile clinics, to help bring care directly to unsheltered people..
3. Insights gained from COVID-19. The pandemic made the relationship between homelessness and health status starkly clear. People experiencing homelessness, especially those in crowded shelters, were at high risk of contracting and suffering complications from COVID-19. In response, the state developed Project Roomkey, an innovative program that aimed to limit the spread of the virus by offering shelter in vacant hotels and motels, thereby protecting people’s health and minimizing strain on the health care system.
While Project Roomkey was meant primarily for people with preexisting health conditions and older adults experiencing homelessness, homeless services staff at the Roomkey sites were surprised by how medically frail many participants were. Upon realizing just how many health services and supports were needed to keep their clients safe and well, they rapidly formed new partnerships with health care organizations to effectively meet residents’ needs. An independent evaluation showed that 62,000 Californians were served through Roomkey.. The report found that the longer people stayed at a Roomkey site, the less likely they were to experience homelessness again — and the more likely they were to move into permanent housing. Project Roomkey proved that if people are given temporary housing that offers privacy, autonomy, and access to necessary services, health and stability can follow. This approach now serves as a national model.
Cross-sector partnerships flourished to help meet this need.
Aiming to Accelerate Momentum Through Grantmaking
At CHCF, we know that developments can stall or take significant time before they are brought to scale. That’s why we are striving to accelerate current momentum through grantmaking. One strategy is to support existing health and homeless sector partnerships while sparking new ones, as with our Partnerships for Action: California Health Care & Homelessness Learning Collaborative. This initiative supports cross-sector pilot projects focused on improving care delivery for people experiencing homelessness.
Another approach is to support interventions outside of the traditional health care system — such as street medicine, medical respite care, and sobering centers — that seek to improve health and housing outcomes.
The common thread across all our homelessness and health care grants is a desire to connect fragmented systems to provide responsive, comprehensive, high-quality care that tackles the full range of health and social challenges in equitable ways.
When I think back to my days as a new doctor, I wonder what became of those first patients who taught me so much. Would their lives be different if they had access to a coordinated set of systems working to support their health and housing needs? Imagining that the answer is ‘yes’ keeps me motivated and helps me dream big.
I’m also inspired by the stories of unhoused Californians I’ve met who have achieved stability because providers of homeless services and health care worked together. At CHCF, we believe that people with lived experiences of homelessness should be compensated partners in the creation and evaluation of policies and practices that affect their lives — people like Lawrence Lincoln, an adviser in our Partnerships for Action learning collaborative.
Lincoln battled trauma, poverty, and addiction for years on the streets of West Oakland before connecting with a street medicine team from Alameda County Health Care for the Homeless. Thanks in part to the organization’s connections to social service, substance-use treatment, and housing navigation providers, Lincoln is now permanently housed, sober, and working as a powerful advocate for street medicine and patient-centered care.
There are thousands more Lawrence Lincolns out there. By continuing to build on California’s movement toward whole-person care, I believe we can reach them, help them achieve the futures they want, and make progress toward a world where homelessness is both rare and brief.
Authors & Contributors





