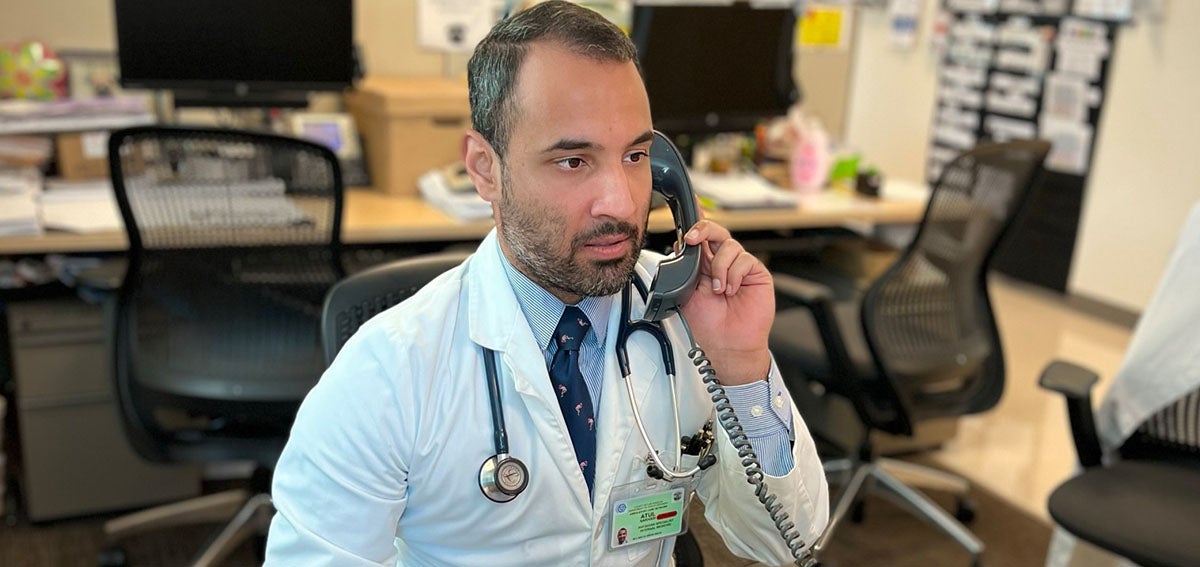
A patient was on the phone with Atul Nakhasi, MD, internist at Martin Luther King, Jr. (MLK) Outpatient Center in Los Angeles, after a routine surgery in the summer of 2021. She was recovering well, and she didn’t want anything to mess with that. The vaccine for COVID-19 might, she thought.
Similar to the hundreds of conversations he’s had with other patients, staff, friends, and strangers, Nakhasi told her the vaccine was not only very safe and would not impair her recovery, but it would also help save her life.
In recent months, an overwhelming majority of patients hospitalized with COVID-19 in Los Angeles County’s four safety-net hospitals were unvaccinated, he told her. The patient listened to him describe the reality on the ground, but she was still unsure, asking questions and reckoning with her choice.
“If you’re vaccinated you’re at least protected from severe sickness or dying from COVID,” Nakhasi said, his voice infused with concern for his patient.
She was quiet. A few seconds of silence hung between them over the call.
Then she said she would get the vaccine but would go to the pharmacy close by.
“That’s great. As a next step, can you set a date and time that works best for you and please update me?” he asked, quietly elated by her transition to yes.
Even before the pandemic came along, patients at MLK Outpatient Center, which serves Compton and Watts and is one of 24 county health centers that are part of the Los Angeles County Department of Health Services, faced the greatest challenges in terms of health outcomes and the largest disparities in LA County. Almost 50% of the clinic’s patients are Black and 50% are Latinx. Eighty percent make under $18,000 per year.
The patient called Nakhasi after receiving her first dose of the vaccine and filled him in on her appointment for the second.
“We’ve learned that it’s just one conversation at a time that can save a patient’s life,” said Nakhasi.
“How I’m saying it is just as important as what I’m saying”
What part of this patient-doctor conversation tipped her over from being apprehensive about the vaccine to accepting?
Nakhasi believes it wasn’t just the information he shared.
“It’s easy to think, ‘Let me just say the facts as a physician, and the individual should come around to yes.’ That oftentimes doesn’t work.”
Instead, he believes on-the-fence patients can be moved to change their minds based on feeling understood and by the emotion in his voice, not just by the information alone.
“When my patients hear my voice of genuine worry and authentic concern, which is so intangible, it emotionally connects with them,” said Nakhasi. “The sense of urgency and importance is conveyed, and patients often respond back with an introspective pause.”
Those few seconds of a silent, reflective pause from a patient have become common enough in conversations that they now signal to Nakhasi that his words have resonated. It’s the moment when patients often rethink their unvaccinated status.
He’s learned that “how I’m saying it is just as important as what I’m saying” when it comes to sharing accurate vaccine information with patients.
Carefully Constructed Conversations
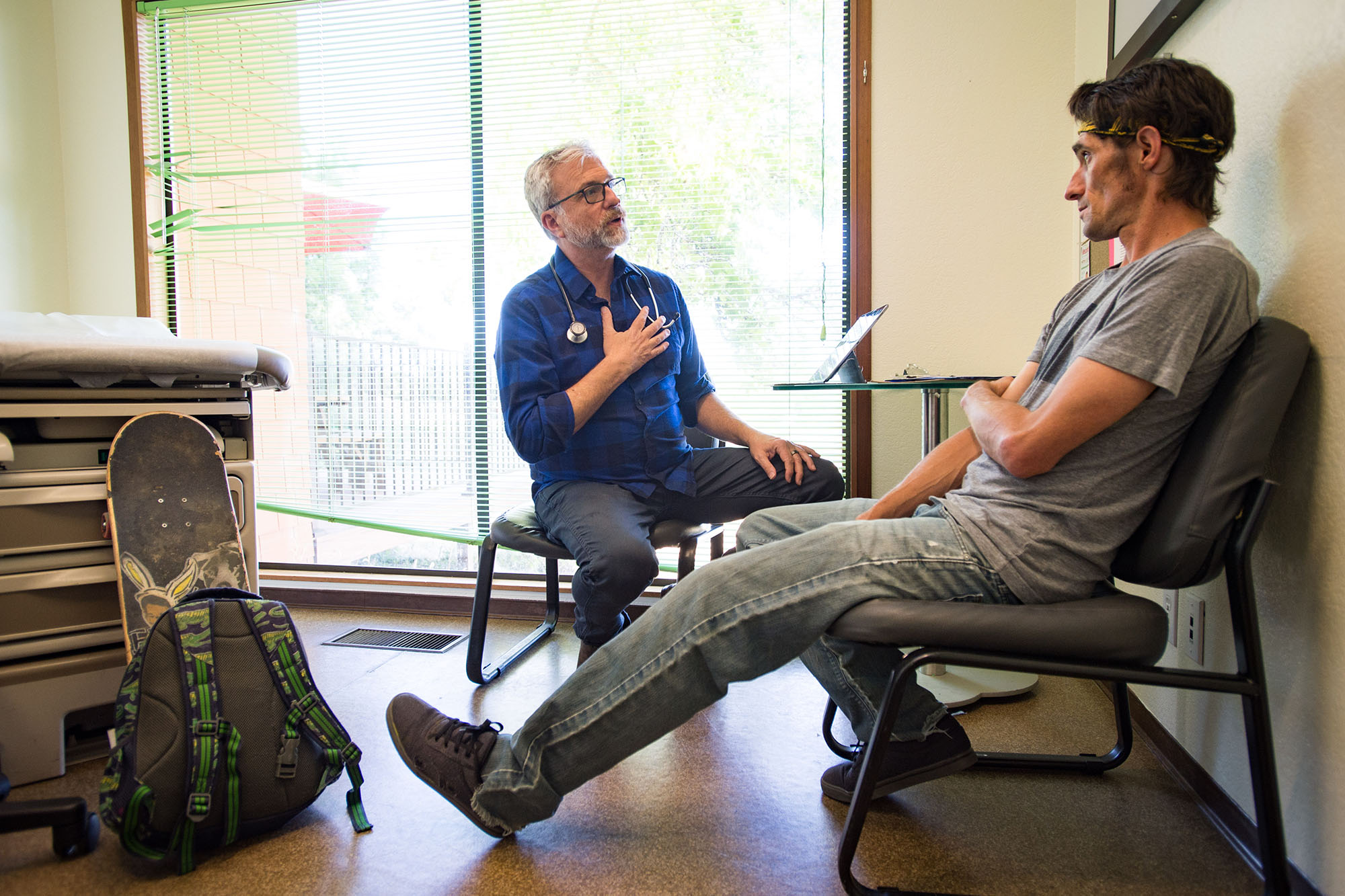
What to share with patients unsure about the vaccine varies, as they are not a monolith. “I can see nine patients in a session and every patient will have a different story” about why they’re unsure about getting the vaccine, said Tasha Dixon, MD, MPH, family medicine lead physician at MLK Outpatient Center.
“We’ve learned that best practice starts with listening and understanding where their concerns and legitimate fears and questions are coming from,” said Nakhasi.
If he begins these high-stakes and delicate conversations with science and data instead, he said, “This backfires because you haven’t really acknowledged a patient’s concerns in a very personal way.”

He’s found that many of those concerns are rooted in patients feeling that their health will worsen with the vaccine. Many have chronic conditions. “The number one thing patients are concerned about is safety,” he said. “Many have a greater fear of the vaccine than the virus. They feel the vaccine may do something harmful to their bodies. They are very concerned about side effects.”
“I take too many medications” is something Dixon regularly hears when she talks with patients about their reticence to get the vaccine. However, she sees this concern as an opportunity.
“This is a perfect setup to say actually that’s exactly why you need the vaccine because you’re already at an increased risk for severe illness,” she said, noting how this approach has helped transition many patients to yes.
A motivational interviewing technique that has also proven effective at MLK Outpatient Center is to ask patients, “On a scale of 1 to 10, how likely are you to get the vaccine?”
“A patient might say, ‘I’m a 3 out of 10,’” Nakhasi explained. “And I’ll ask, ‘How come you’re not a one?’ This helps unlock their reason and personal motivation to potentially getting vaccinated.” This information enables Nakhasi to more specifically tailor his messages so they have a higher chance of resonating with the patient.
To date, health care workers are making progress, yet it can sometimes be a slow process and a heavy lift to further increase vaccine uptake.
History, Motives, and Mistrust
The historical institutional racism and trauma that led Black and Latinx communities to mistrust that the medical system works in their best interests have also driven skepticism about vaccines.
“A lot of what I’ve heard has been, ‘They’re not going to give me a shot in my arm when I don’t know what’s in it,’” said Dixon.
Some of what patients tell her today also reminds her of what she heard growing up: Doctors are only out to make money. You can’t trust them.
Some patients suspect Dixon and other physicians want to administer the vaccine so they can enrich themselves. “None of us are getting paid for this,” she tells patients. “What we took an oath to do is to save lives and to do no harm.”
She understands, though.
“As someone who grew up in an African American household in the inner city of Dallas, Texas, I empathize,” said Dixon. “I didn’t grow up seeing a doctor, so I completely understand their rationale as to why they don’t necessarily trust us or why someone is a little bit leery.”
She finds it effective to let patients know that what she’s telling them about the vaccine is exactly what she tells her own family. Dixon said this sets the stage for an open and honest conversation where she can hear a patient out while dispelling misinformation.
She also plans to build familiarity and trust with those in the community who “don’t know what a clinic looks like or are afraid of the idea of seeing a doctor” by providing tours of MLK Outpatient Center.
“When you come in, you will realize it’s not so bad. You will give us a chance to take care of your health.” And this will give Dixon a chance to have the vaccine conversation.
“Journey of Trust”
“Changing a patient from a no to a yes is not an overnight process, and it does become frustrating and disenchanting when the patient continuously says no,” said Dixon. “I tell patients, ‘You can always tell me no, but my job is to make sure you have all the information that you need.’”
“Most times, I don’t get to yes in the first conversation,” said Nakhasi, who describes patients needing reassurance and time to process.
He’s found that it helps to write where the vaccine conversation with the patient left off in their medical record, so he can quickly pick it up the next time they speak.
“I often say it’s like a football field. You might start at your own 10-yard line, but it’s a journey to move the ball a little bit further down the field. It might be three or four conversations to get to the end zone.”
Nakhasi believes this “journey of trust” to vaccine acceptance boils down to the bond between patient and physician.
“There’s certainly a lot of rightful mistrust of institutions,” he said. “But the personal relationship to people’s own doctor, not just some doctor on TV, but their own personal doctor who has found their cancer and helped treat it, who has taken care of their mother, who has saved their limb from diabetes? And that same doctor is now advocating for them to get the vaccine to protect their life? That’s the difference,” and why he believes his long-standing patients listen and trust in him.
Patients as Trusted Messengers
People also listen to what family and friends tell them about the vaccines. “A critical insight has been that patients are trusted messengers to their own family members,” Nakhasi said. These messengers are in addition to the staff and community health workers who have been trained in the conversational techniques that Nakhasi and Dixon employ.
In hopes of expanding these conversations to more people, providers and health care workers have been asking their vaccinated patients to talk with unvaccinated family and friends. Nakhasi tells them that such a conversation about getting vaccinated “could save your mom’s life. It could save your brother’s life. It could save your child’s life.” He recently vaccinated a nurse who brought her children — a teenager and a young adult — to MLK Outpatient Center to receive the shot.
Dixon also encourages her vaccinated patients to let their loved ones know they can walk into the clinic — no appointment or medical card needed — to get their shot for free. “We are vaccinating anyone and everyone,” she tells them.
“We can’t do this alone,” Nakhasi said of the patients-as-trusted-messengers approach.
The Hard Noes
What about those patients who are hard noes? “A no today may mean a yes in three months or a yes tomorrow, so we keep trying to address their concerns. I keep telling them, ‘I’m not going anywhere.’ I am not giving up on this fight,” said Dixon.
“Most people still want to do what’s right for themselves, so I have an overriding sense of optimism,” said Nakhasi about the ongoing drive toward vaccination.
However, the darker moments also motivate him. “I was in with a patient when a nurse knocked on my door and said, ‘You need to sign this.’ I looked down and it was the death certificate of one of my own patients. And I was shocked that this patient didn’t make it. I think if they had the vaccine, they would still be with us in this world. That keeps me going.”
This article was first published by the California Association of Public Hospitals and Health Systems (CAPH) on October 27, 2021, and is reprinted with permission of CAPH and the author. Copyright 2021, all rights reserved.
This is one of a series of CAPH blog articles funded by the California Health Care Foundation.
Authors & Contributors

Aisling Carroll
Aisling Carroll is a Bay Area–based freelance writer and former journalist who covers health care, digital health, hospitals, and the patient-doctor relationship. Her work has been published in Stat News, HuffPost, Business Insider, Congressional Quarterly, and others. Carroll received a bachelor’s degree in political science from UC San Diego.