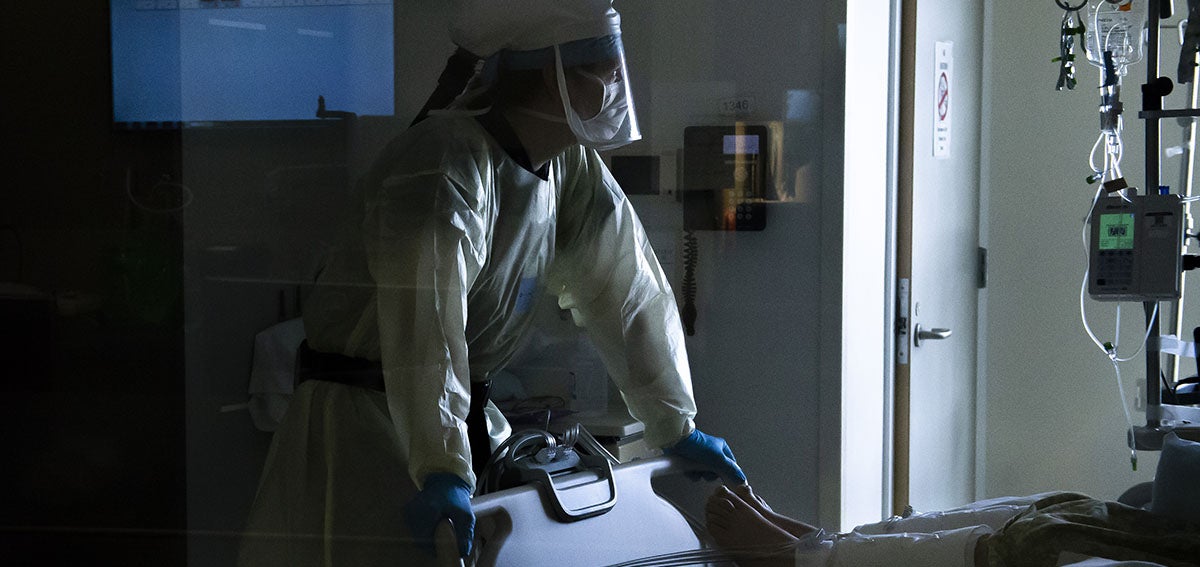
Taylor Nichols, MD — suited up in a mask, face shield, gown, and gloves — stood outside a patient’s room at Mercy San Juan Medical Center in Sacramento County, and he hesitated. An emergency room physician, Nichols was preparing to intubate the man, who was suspected of having an advanced case of COVID-19. Solidly built and struggling to breathe, the man begged, “Don’t let me die, Doc.” Nichols treats such patients daily, but this one was different. Nichols saw the man had multiple Nazi symbols tattooed on his body, including a prominent swastika on his chest.

Nichols is Jewish, and that day he was working alongside a Black nurse and an Asian respiratory therapist. Together, they were about to perform one of the riskiest procedures of the COVID-19 era. Intubation exposes health care workers to aerosols and droplets from an infected patient’s airways.
“The symbols of hate on his body outwardly and proudly announced his views,” Nichols wrote on Twitter. “We all knew what he thought of us. How he valued our lives.”
In his moment of hesitation, Nichols realized that he didn’t feel compassion for the patient. “The pandemic has worn on me,” he wrote. “All this time soldiering on against the headwinds.”
In every region of the US, emergency rooms and intensive care unit (ICU) beds are filling up with seriously ill COVID-19 patients as never before. But on this third surge of the pandemic, health care workers — “the most precious resource the US health care system has in the struggle against COVID-19” — are physically and mentally exhausted, Ed Yong wrote in the Atlantic. “In the imminent future, patients will start to die because there simply aren’t enough people to care for them.”
What the Breaking Point Looks Like
Jahan Fahimi, MD, an emergency care physician at UCSF and a mentor to Nichols, told the San Francisco Chronicle’s Jill Tucker that Nichols is one of the most passionate, mission-driven physicians he knows. “If you can break Taylor, then something horrible has happened,” Fahimi said. “I wonder how we are going to sustain [health care providers] for a number of more months.”
A study of the mental health toll of COVID-19 on frontline health care workers in New York City during the first surge last spring substantiates Fahimi’s concerns. Researchers surveyed 657 workers at a large medical center during a spike in inpatient admissions for COVID-19 and found that 57% of participants screened positive for acute stress, 48% for depressive symptoms, and 33% for anxiety. Nurses and advanced practice providers fared worse than attending physicians or medical residents/fellows: 64% screened positive for acute stress, 53% for depressive symptoms, and 40% for anxiety.
“To be a nurse, you really have to care about people,” Whitney Neville, a registered nurse in Iowa, told Yong. But when the onslaught of COVID-19 patients becomes unbearable, “to protect yourself, you just shut down. . . . There’s only so many bags you can zip.”
California Ill-Prepared
As recently as October, California was praised by medical and public health experts for its handling of the coronavirus. For its size and population, the state appeared to be controlling virus transmission and hospitalizations.
But with just weeks left in 2020, the tide has turned. On December 6, the California Department of Public Health reported 30,075 new COVID-19 cases, a new daily record. Over 10,600 Californians have been hospitalized with COVID-19, and 75% of the state’s ICU beds are occupied. Without intervention, state ICUs could be overwhelmed by Christmas Eve, Reese Oxner reported for NPR.
Southern California has been hit especially hard. Los Angeles County, which reported a record 10,528 new positive cases on December 6, faces “one of the most dangerous moments in this pandemic,” Barbara Ferrer, director of the Los Angeles County Department of Public Health, said in a recent briefing.
In Riverside County, which saw daily positive cases jump 22% in 14 days, Eisenhower Health has initiated virtual counseling for nurses to address the emotional burden of caring for the nonstop stream of COVID-19 patients, Maria La Ganga and Brittny Mejia reported in the Los Angeles Times. “The entire team is emotionally fatigued from this marathon,” said Tina Wallum, director of critical care units and inpatient dialysis at Eisenhower. “I have never seen anything like this in my nursing career. These patients are some of the sickest patients I’ve ever seen.”
In a recent CHCF survey of California health care providers, between one-half and two-thirds of providers said they feel emotionally drained, frustrated, overworked, and burned out. California’s health workforce shortage has come to a head during the pandemic, Kristof Stremikis, director of CHCF’s Market Analysis and Insight team, told the New York Times. “The system is blinking red when it comes to the workforce,” he said. “We don’t have enough of many different types of clinicians in California and they’re not in the right places.”
Preparing for the Worst Case
Hospitals across the country are prepping for the worst-case scenario even as significant delays in state data reporting over the Thanksgiving holiday temporarily obscured trends.
The University of Cincinnati Health hospital system recently converted its cardiovascular recovery unit into surge ICU capacity, Peter Sullivan reported in the Hill. Rhode Island and Wisconsin are among states that have readied field hospitals to take overflow patients, Tammy Webber and Heather Hollingsworth reported in the Associated Press (AP).
But even states that have enough hospital beds may not have enough staff to care for patients. “You can’t just say we’ll have doctors and nurses from other states come because those other states are also dealing with COVID patients,” Amesh Adalja, MD, an infectious diseases expert at Johns Hopkins University, told the AP.
Provider shortages nationwide have been compounded by doctors and nurses retiring early or leaving their jobs because of pandemic stress. Nearly one in five primary care clinicians (PDF) surveyed in September by the Larry A. Green Center and Primary Care Collaborative said COVID-19 has prompted someone in their practice to retire early or to plan to do so.
Many people working in medical practices are worried about financial stability. Seventy-four percent of clinicians surveyed by the Larry A. Green Center reported working without pay for 6 to 20 hours a week, and 7% of clinicians said they were unsure their practice could remain open past December without financial assistance. A survey conducted by the California Medical Association found that 87% of California physician practices were worried about their financial health (PDF).
“You can’t see the impact right away, but I think if we look three or four years down the line, we will find that our primary care shortage is worse because of the pandemic,” Yalda Jabbarpour, MD, medical director of the Robert Graham Center for Policy Studies, affiliated with the American Academy of Family Physicians, told Roz Plater in Healthline.
Even though caring for COVID-19 patients has taken a mental health toll on Nichols, he still loves his chosen profession. He doesn’t know whether the tattooed patient ultimately lived or died, but Nichols and his team worked to make sure they gave him the best chance of survival that they could.
“I think I’ll be OK,” he told the Chronicle. “I don’t know if I am now.”
The Frontline Workers Counseling Project is providing free mental health counseling to frontline and essential workers in the Bay Area and nearby counties. The California Medical Association’s Care 4 Caregivers Now initiative has free and confidential peer coaching from trained medical practitioners. Finally, if you or someone you know is in distress, please call the 988 Lifeline at 988. Free and confidential emotional support is available through the lifeline 24/7.
Authors & Contributors






