The growth of Medi-Cal since the Affordable Care Act (ACA) has been widely discussed: The program now covers more than 13 million Californians, primarily children, adults, and seniors with low incomes as well as people with disabilities. Less often discussed, however, is how Medi-Cal’s expansion has affected access to care for those it covers. The answer has important ramifications for California’s next steps in expanding coverage to the state’s approximately three million remaining uninsured people.
On January 17, I had the opportunity to address this question before the Assembly Select Committee on Health Care Delivery Systems and Universal Coverage, which is exploring options for moving California toward universal coverage. Below is a summary of the key points from my presentation along with selected slides. Because children represent only 3% of California’s remaining uninsured, I focused my presentation on adults. (You can download my presentation, and a video of my testimony follows this article.)
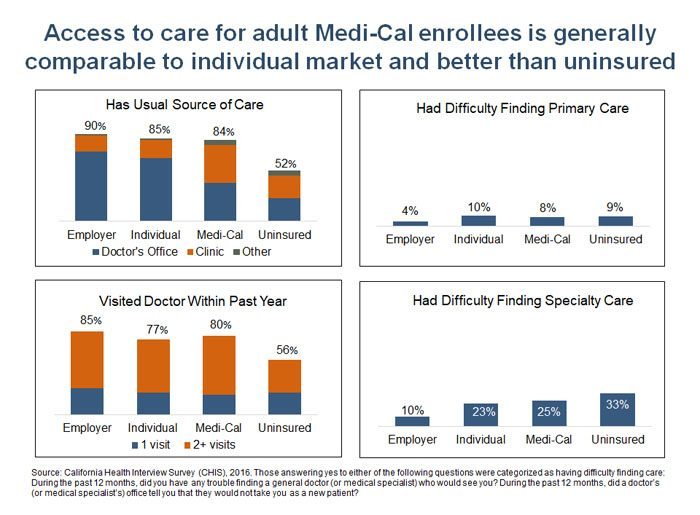
1. Access to care for adult Medi-Cal enrollees is generally comparable to those in the individual market and better than that for the uninsured.
The California Health Interview Survey (CHIS) measures access to care in a variety of ways, and some of its important findings are shown in the slide below. Access for Medi-Cal enrollees is comparable to those in the individual market, and better than that for the uninsured. However, the data also show a notable disparity between Medi-Cal and employer coverage, which has been observed in previous studies.
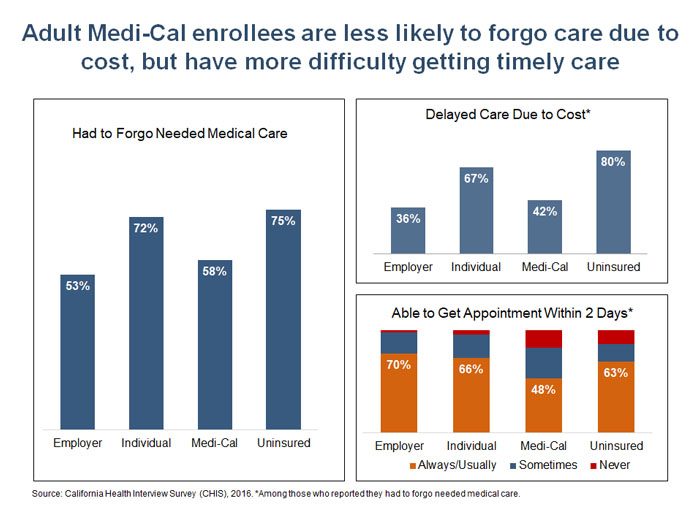
2. Adult Medi-Cal enrollees are less likely to forgo or delay care due to cost, but they have more difficulty getting timely care.
Additional CHIS measures show that Medi-Cal enrollees experience fewer financial barriers to care compared to both the uninsured and people in the individual market. This is not surprising given that Medi-Cal has no (or very low) premiums and copays. However, Medi-Cal enrollees report far more difficulty than any other coverage group in getting a needed appointment within two days.
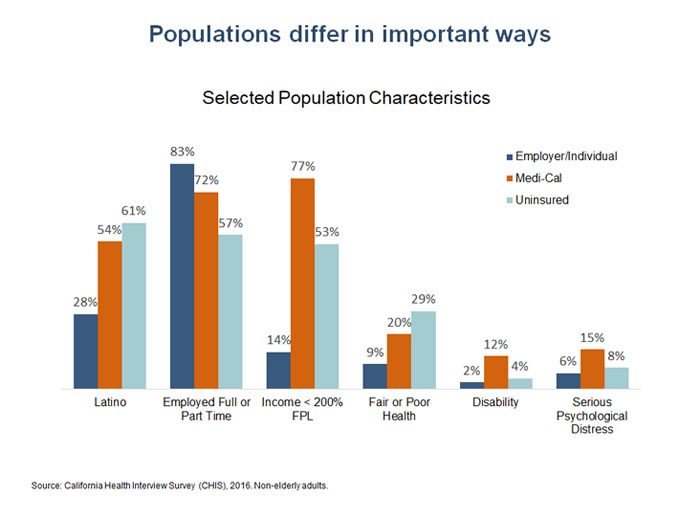
3. Underlying characteristics of the Medi-Cal population partly explain some of the disparities in access.
Comparing Medi-Cal to other sources of coverage can provide a useful benchmark for determining whether Medi-Cal enrollees have equal access to care, as required under federal law. However, it’s also important to consider the underlying characteristics of the populations being compared — some of which are associated with better access and some with worse — regardless of the type of coverage. For example, people in poor health or who have a disability often experience greater difficulty accessing care than those in good health irrespective of their source of coverage. Higher rates of poor health, disability, and mental distress are a few of the many differences between the Medi-Cal population and other insured Californians.
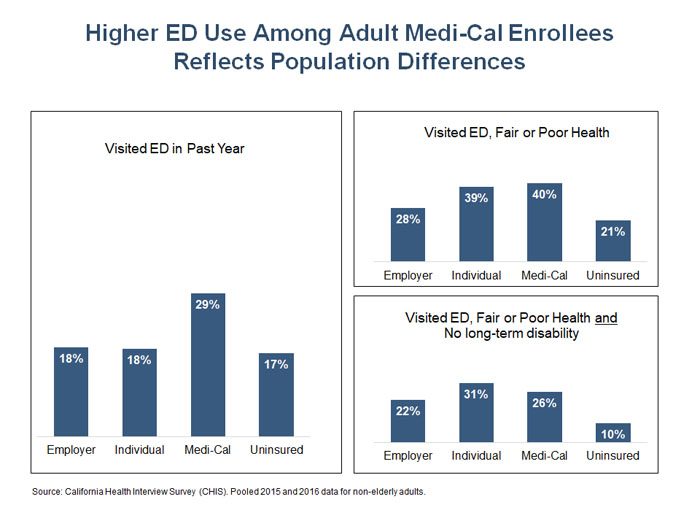
In general, Medi-Cal enrollees are more likely to visit the emergency department than those with other types of coverage or the uninsured — a fact that has received a lot of attention lately. However, the gap between Medi-Cal and other insured groups shrinks once health status is considered, and it shrinks further when both health status and disability are factored in.
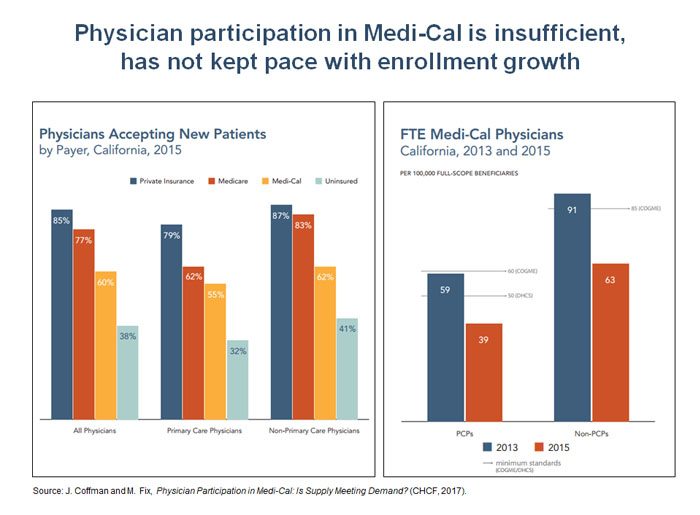
4. Not enough doctors accept Medi-Cal, contributing to access challenges.
While population characteristics explain some of the disparities in access to care for Medi-Cal enrollees, there also are conspicuous delivery system challenges that contribute to the problem.
A CHCF-funded study conducted by the University of California, San Francisco (UCSF), found that while there was an increase in provider participation in Medi-Cal under the ACA, it was not enough to keep pace with the surge in program enrollment. As a result, the ratio of participating providers to full-scope enrollees in the Medi-Cal program (excluding those with emergency Medi-Cal coverage) fell between 2013 and 2015 and is now well below state and federal guidelines. The UCSF study showed that California’s physicians are less likely to accept new Medi-Cal patients than patients on Medicare or private insurance. However, physicians were still more likely to accept new Medi-Cal patients compared to uninsured patients.
5. Payment rates are the top reason why physicians report they don’t participate in Medi-Cal.
In the same survey, physicians indicated that payment rates were the top reason for limiting their participation in Medi-Cal. Physicians also expressed great frustration at what they perceived as the administrative burdens of participating in Medi-Cal and the difficulty in obtaining specialty referrals for their patients.
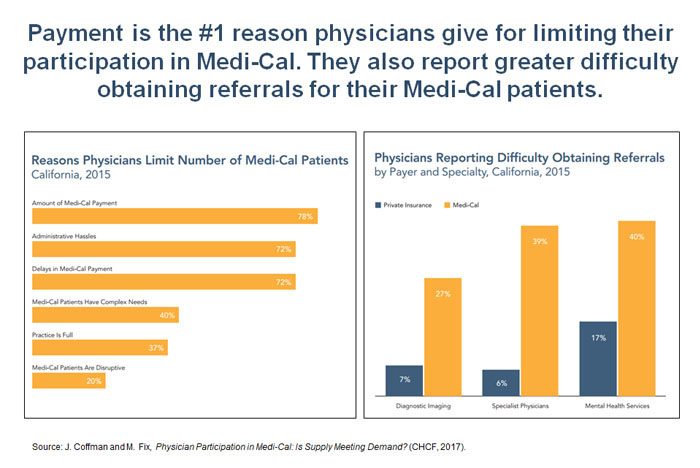
It’s worth noting that this survey question did not distinguish between Medi-Cal fee-for-service rates, which are known to be among the nation’s lowest (on average), and rates paid by Medi-Cal managed care plans, which are not publicly available. Because managed care plans now cover about 90% of full-scope Medi-Cal enrollees, a reasonable interpretation of the response to this question is that physicians’ dissatisfaction with both fee-for-service and managed care rates is contributing to low rates of participation in Medi-Cal.
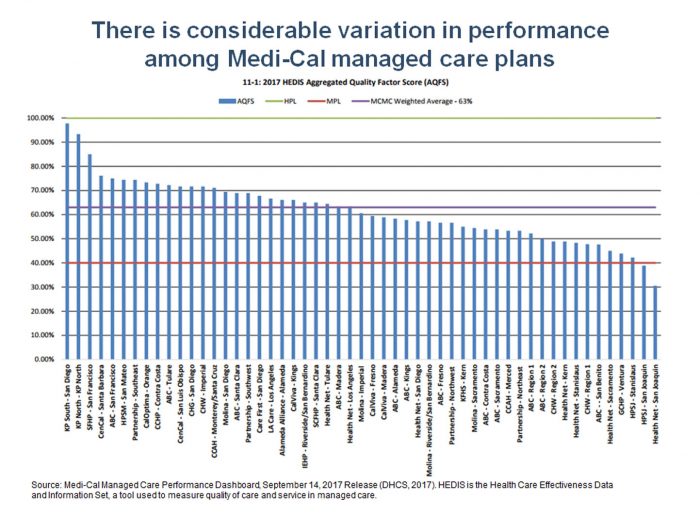
6. Medi-Cal managed care plans are key players in improving access.
How is managed care doing? The chart below is from the Department for Health Care Services Medi-Cal managed care performance dashboard, and it shows aggregate quality scores across various measure for each plan. The individual plan names may be difficult to read in this version of the slide (click on it for a larger view), but the main point is clear: Performance varies tremendously across plans. If access and quality were uniformly as good as they are for the top-scoring plans, millions of Californians with low incomes would be better off, getting appropriate and timely preventive and primary care.
7. There are a variety of ways to improve access in Medi-Cal.
I closed my talk with some ideas for improving access based on lessons from our experiences at CHCF and from the work we do with health plans and providers in the safety net. They included:
- Pay plans differently based on performance. There is clearly an opportunity to improve health plan performance. Many organizations have adopted pay-for-performance incentives for providers. Medi-Cal could do the same, paying more to plans that improve access and quality and less to those that don’t.
- Encourage plans to expand access to telehealth. Public health care systems in San Francisco and Los Angeles have used electronic referral and consultation systems to reduce unnecessary visits to specialists and cut months off appointment wait times. Similarly, telehealth is connecting rural and urban providers with specialists practicing in other parts of the state. A few health plans are investing in telehealth, but there is great room for improvement. Any plan serving rural areas or receiving an exemption from Medi-Cal’s network adequacy or timely access requirements should have a robust telehealth program in place.
- Expand delivery system reforms funded through federal Medicaid waivers to Federally Qualified Health Centers (FQHCs). Through federal waivers, Medi-Cal has invested billions in the transformation of care delivered by public, University of California, and district hospitals, and in the state’s system for addressing substance use disorders. Such efforts, which are essential to building the system capacity we need now and in the future, should continue and expand to FQHCs and other types of providers that deliver primary care to large numbers of Medi-Cal patients.
- Invest in building a health care workforce for the future. This workforce should emphasize patient-centered, team-based care. The California Future Health Workforce Commission, with strong support from CHCF and many other funding partners, will issue recommendations in 2018, and I hope they will be widely discussed and acted upon.
- Expand the tracking of network adequacy and timely access. Greater accountability, including better, more accurate, and more timely data on network adequacy and timely access to care, are sorely needed. Current efforts by the California Department of Managed Health Care and the state Department of Health Care Services to advance better measurement and greater transparency around network adequacy and timely access should be expanded.
The experience of Medi-Cal enrollees gives us reasons to celebrate the progress we’ve made in covering millions of previously uninsured Californians and also to roll up our sleeves and ensure that all Medi-Cal enrollees have access to the timely, high-quality, and patient-centered care we all need.
Authors & Contributors






